

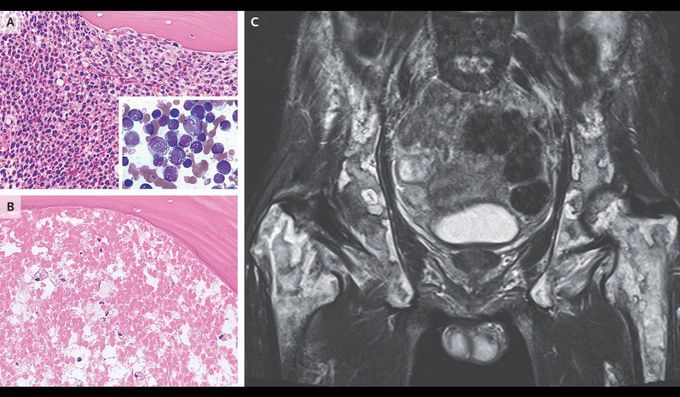
Bone Marrow Necrosis in Acute Monoblastic Leukemia
A 56-year-old man presented to an outpatient clinic with a 7-day history of fever, mild fatigue, and shortness of breath. On physical examination, his abdomen was nontender and distended, with hepatomegaly and splenomegaly, and cervical lymphadenopathy was noted. Laboratory studies revealed a white-cell count of 142,000 per microliter (reference range, 3500 to 9800) with 92% monoblasts, a hemoglobin level of 7.6 g per deciliter (reference range, 13.5 to 17.5), and a platelet count of 36,000 per microliter (reference range, 130,000 to 370,000). A bone marrow biopsy revealed leukemic infiltration of the marrow with monoblasts (Panel A, bone marrow specimen stained with hematoxylin and eosin; inset, aspirate smear stained with May–Grünwald–Giemsa). A diagnosis of acute monoblastic leukemia was made, and the patient received induction chemotherapy. Diffuse alveolar hemorrhage and acute kidney injury subsequently developed in the context of disseminated intravascular coagulation and tumor lysis syndrome. After the patient’s condition improved, he began having persistent lower back pain. Pelvic bone marrow specimens showed diffuse ghost cells indicative of necrosis (Panel B). Magnetic resonance imaging of the pelvis revealed areas of high and low signal intensity that had a marble-like appearance, findings that suggested necrosis of hematopoietic and stromal elements (Panel C). The patient underwent allogeneic stem-cell transplantation; however, the leukemia recurred and he died 4 months later.

