

Cold Agglutinin Syndrome
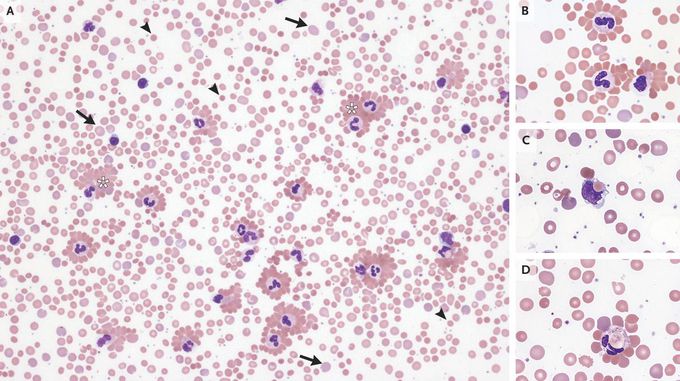
A 3-year-old girl presented to the emergency department with a 1-day history of dark urine and jaundice after the development of an upper respiratory tract infection 1 week earlier. The physical examination was notable for pharyngeal erythema and exudates, conjunctival pallor, and scleral icterus. There was no hepatosplenomegaly, rash, or acrocyanosis. Laboratory studies showed a new anemia and findings consistent with hemolysis. A subsequent peripheral-blood smear (Panel A) showed varied sizes and shapes of red cells that included reticulocytes (arrows) and spherocytes (arrrowheads), as well as erythrocyte agglutination (asterisks). Many neutrophils were coated with agglutinated erythrocytes, forming rosettes (Panel B). Phagocytosis of erythrocytes in macrophages (Panel C) and neutrophils (Panel D) was also seen — rare findings in autoimmune hemolytic anemia. A direct antiglobulin test was positive for C3d and weakly positive for IgG. The cold agglutinin titer was 1:1024. Tests for Mycoplasma pneumoniae, Epstein–Barr virus, and other common respiratory viruses were negative. A diagnosis of autoimmune hemolytic anemia from cold agglutinin syndrome associated with an upper respiratory infection was made. Supportive care, including blood transfusions and cold avoidance, was provided. At the 3-week follow-up, the child felt well and the anemia had abated.

