

Treatment of internal derangement
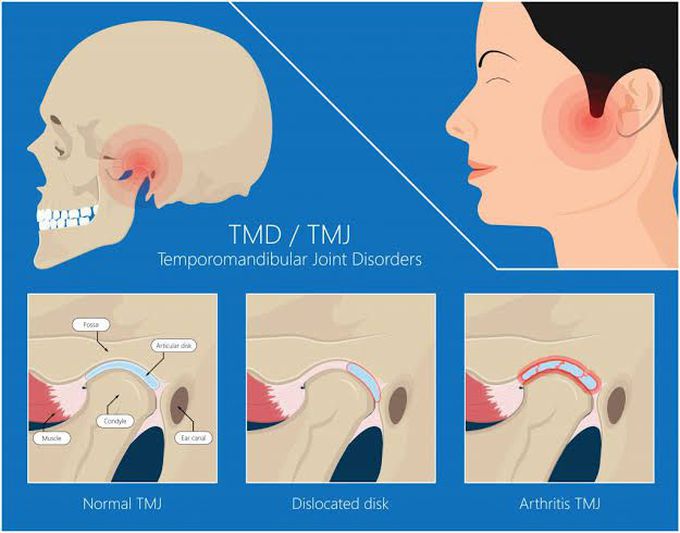
Diagnosis of disk derangement with reduction requires observation of the jaw when the mouth is opened. When the jaw is opened > 10 mm (measured between the incisal edges of the upper and lower incisors), a click or pop is heard, or a catch is felt, as the disk pops backward over the head of the condyle. The condyle remains on the disk during further opening. Usually, another, more subtle (reciprocal) click is heard during closing when the condyle slips over the posterior rim of the disk and the disk slips forward. Diagnosis of disk derangement without reduction requires that the patient open as wide as possible. The opening is measured, and gentle pressure is then exerted to open the mouth a little wider. Normally, the jaw opens about 45 to 50 mm; if the disk is deranged, it will open about ≤ 30 mm and the jaw will deflect to the affected side. Closing or protruding the jaw against resistance worsens the pain. MRI is sometimes done to confirm presence of a disk derangement (by observing the position of the disk relative to the condyle during opening and closing) or to determine why a patient is not responding to treatment. Capsulitis is often diagnosed based on a history of injury or infection along with exquisite tenderness over the joint and by exclusion when pain remains after treatment for myofascial pain syndrome, disk derangement, arthritis, and structural asymmetries. However, capsulitis may be present with any of these conditions.

