

Orbital Apex Syndrome
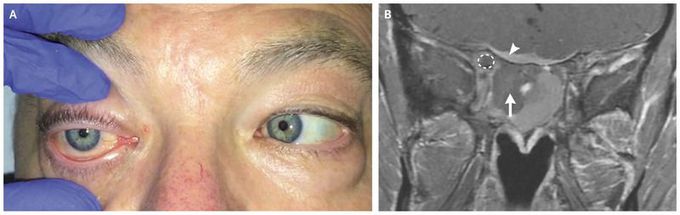
A 61-year-old man presented to the emergency department with a 3-week history of right retro-orbital pain and a 1-week history of double vision, lid droop, and loss of vision. Ophthalmologic examination revealed reduced vision in the right eye (only hand motion was perceived), a relative afferent pupillary defect, a poorly reactive pupil, and near-complete ophthalmoplegia. Loss of sensation in the cornea, upper eyelid, and forehead confirmed neuropathies of cranial nerves II, III, VI, and V1. T1-weighted magnetic resonance imaging with contrast revealed proptosis with infiltration of the orbital apex. A coronal view (Panel B) showed a heterogeneous fluid signal between the sphenoid sinuses, which later proved to contain mucus, blood, and necrotic material on the right (arrow). Soft-tissue infiltration within the orbital apex circumscribed the right optic nerve (dashed circle) and was seen in the adjacent dura (arrowhead). A diagnosis of orbital apex syndrome affecting the right eye was made. Orbital apex syndrome can result from multiple causes, including neoplasia, trauma, inflammation, and infection. The syndrome manifests as visual impairment from optic nerve dysfunction combined with extraocular muscle palsy. The patient underwent endoscopic sinus surgery with orbital apex decompression, and a biopsy specimen was obtained. The surgical procedure, in addition to treatment with glucocorticoids, improved visual acuity in the right eye to 20/70. Pathological analysis of the biopsy specimen revealed high-grade, diffuse, large B-cell lymphoma, and findings from further studies showed widespread disease. Chemotherapy was initiated; however, the patient died 6 weeks later.

