

Acquired Reactive Perforating Collagenosis
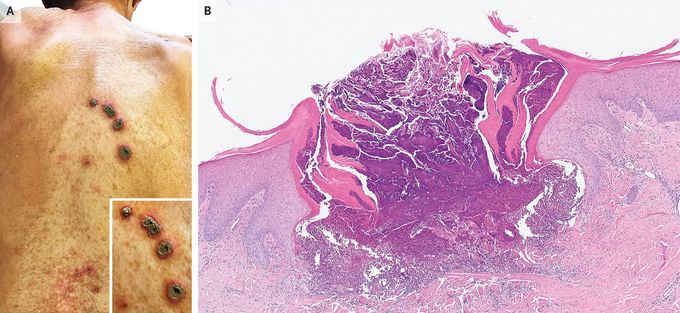
An 83-year-old woman with a history of type 2 diabetes mellitus presented to the dermatology clinic with a 4-month history of an itchy rash on her back. One year before presentation, her glycated hemoglobin value had been 8.5%. On physical examination, there was a linear array of crateriform lesions containing crusted material on an erythematous base on her mid-upper back (Panel A, inset), as well as several similar but smaller lesions on her lower back (Panel A). Routine serum laboratory tests were normal. A skin biopsy from a small lesion on the upper back revealed a cup-shaped ulceration with transepidermal elimination of basophilic collagen and with cellular debris (Panel B, hematoxylin and eosin stain). A diagnosis of acquired reactive perforating collagenosis was made. Acquired reactive perforating collagenosis is a perforating dermatosis — a skin condition in which dermal connective tissue “perforates” through the epidermis. Acquired reactive perforating collagenosis is associated with underlying systemic conditions (e.g., diabetes, as in this patient). Treatment involves addressing the underlying condition and reducing pruritus, which probably triggers the development and perpetuation of the skin disease. Treatment with topical glucocorticoids and keratolytic agents, plus systemic antihistamines, was initiated. Five weeks after the initial visit, the patient died from pneumococcal sepsis.

