

Eosinophilic Fasciitis
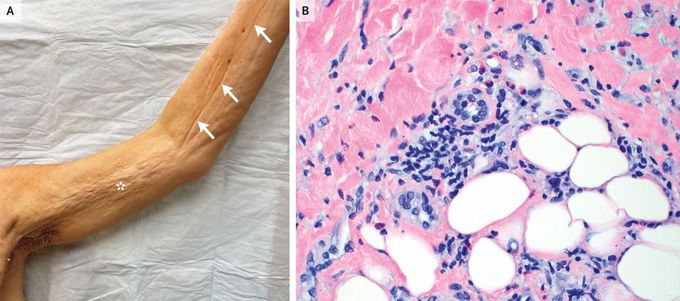
A 66-year-old man presented to the dermatology clinic with an 8-month history of progressively worsening, painful skin tightening and swelling of his arms and legs. He had received treatment for possible scleroderma with oral glucocorticoids and methotrexate, but the symptoms had progressed. On physical examination, there was symmetric, woody induration of the trunk, arms, and legs, sparing the hands and feet. The involved skin had a dimpled appearance (peau d’orange changes) (Panel A, asterisk). Elevation of the arms resulted in visible indentations along the course of superficial veins, a finding known as the “groove sign” (Panel A, arrows). Elbow contractures were also noted. Laboratory studies were notable for an absolute eosinophil count of 2040 cells per cubic millimeter (reference range, 15 to 500) and a normal antinuclear antibody level. A skin biopsy of the left arm was performed. Histopathological examination showed a perivascular and interstitial inflammatory infiltrate of lymphocytes and eosinophils in the deep reticular dermis and subcutis (Panel B, hematoxylin and eosin stain). A diagnosis of eosinophilic fasciitis was made. Owing to the severity of the patient’s symptoms and the lack of a previous response to oral glucocorticoids and methotrexate, treatment with intravenous methylprednisolone, oral mycophenolate mofetil, and intravenous immune globulin was initiated. At 4 months of follow-up, his symptoms had markedly abated.

