

Desquamative Interstitial Pneumonia
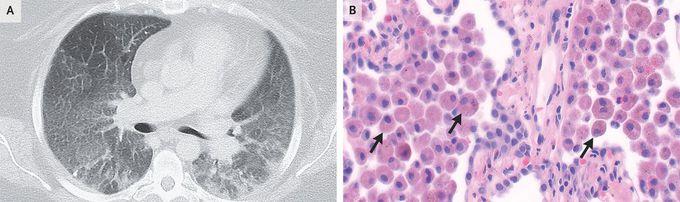
A 34-year-old woman with tobacco use disorder, severe obesity, and chronic hypoxemic respiratory failure of unknown cause was referred to the pulmonary clinic for worsening dyspnea and dry cough. She reported no history of environmental or occupational exposures, substance use, or fevers. Her oxygen saturation was 93% while she was receiving 3 liters of supplemental oxygen. On physical examination, breath sounds were quiet but vesicular. There was no clubbing of the fingers. Pulmonary-function tests showed mild restriction and a mild reduction in diffusing capacity. Computed tomography of the chest showed diffuse ground-glass opacities and areas of peripheral consolidation but no basilar reticulations or honeycombing (Panel A). The results of testing for autoantibodies and hypersensitivity pneumonitis were negative, and bronchoalveolar lavage was not diagnostic, so surgical lung biopsy was performed. The histopathological analysis showed interstitial fibrosis and extensive alveolar filling with pigment-laden macrophages on hematoxylin and eosin staining (Panel B, arrows). These findings were consistent with a diagnosis of desquamative interstitial pneumonia, a rare form of idiopathic interstitial pneumonia that is highly associated with cigarette smoking. A lung biopsy is necessary to make the diagnosis. Treatment with a smoking-cessation program and a tapering dose of glucocorticoids was initiated. At the 3-month follow-up, the patient’s symptoms remained unchanged as she continued to engage in smoking cessation.
Living with Pulmonary Fibrosis (PF) was one of the hardest experiences of my life. The breathlessness, the fatigue, and the fear of the future weighed on me every single day. I had tried so many treatments and medications, but nothing seemed to stop the disease from progressing.Out of both hope and desperation, I came across NaturePath Herbal Clinic. At first, I was skeptical but something about their natural approach and the stories I read gave me the courage to try one more time.I began their herbal treatment program, and within a few weeks, I noticed small changes easier breathing, more energy, and a clearer mind. Over themonths, those improvements became more and more obvious. Today, I can truly say my life has changed. My lungs feel stronger, and my quality of life has returned in ways I didn’t think were possible.This isn’t just a testimony it’s a heartfelt recommendation to anyone struggling with PF or other chronic conditions. Don’t give up hope. I’m so grateful I gave NaturePath Herbal Clinic a chance. Visit their website to learn more: www.naturepathherbalclinic.com info@naturepathherbalclinic.com


