

Acute Ocular Toxoplasmosis
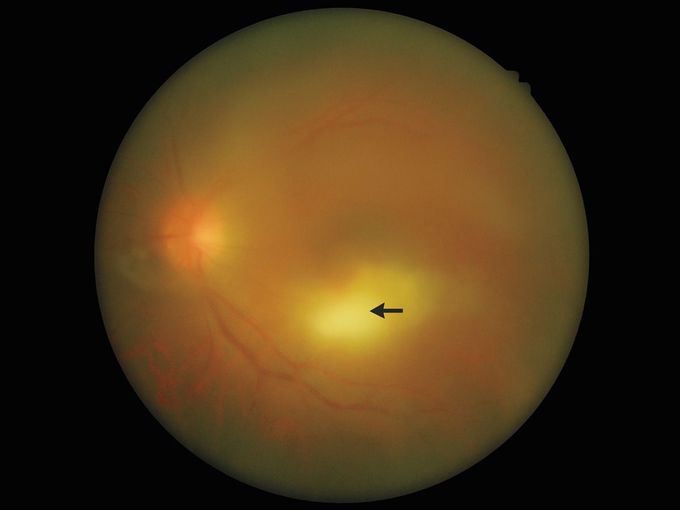
A 49-year-old man presented to the ophthalmology clinic with a 1-week history of blurry vision and glare in his left eye. He had no systemic symptoms. An ophthalmologic examination showed visual acuity of 20/200 in the left eye and mild granulomatous uveitis in the anterior chamber. An ophthalmoscopic evaluation was notable for focal chorioretinitis and moderate vitreous inflammation, the latter of which generated a bright-white reflection — also known as a “headlight in the fog” appearance. The examination of the right eye was normal. A diagnosis of acute ocular toxoplasmosis was made. The patient reported contact with his pet dog but no contact with other animals or with undercooked meats. Ocular toxoplasmosis is the most common infectious cause of posterior uveitis. It may manifest as changes in vision that are accompanied by unilateral chorioretinitis and vitritis, or it may be asymptomatic, in which case chorioretinal scars are later identified incidentally. Ocular toxoplasmosis is a clinical diagnosis, although serologic testing may support the diagnosis in some cases. Treatment with oral antimicrobial therapy and systemic glucocorticoid agents was initiated. At follow-up 1 month later, the vitreous inflammation of the left eye had abated, but the visual acuity remained 20/200.

