

Giant-Cell Arteritis
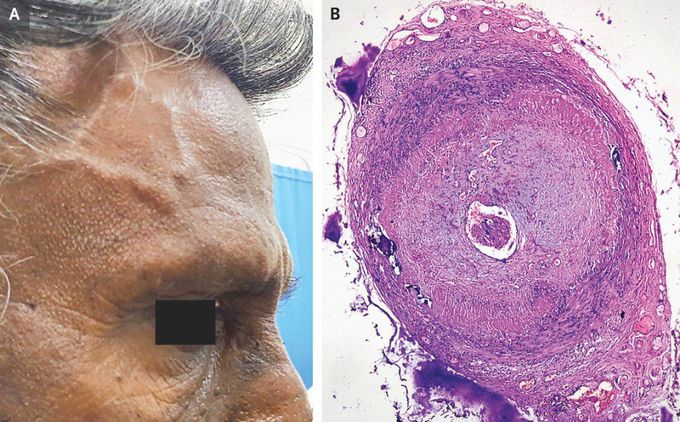
A 70-year-old man presented to the neurology clinic with a 3-week history of temporal headache and jaw pain with chewing. He reported no vision changes. On physical examination, both temporal arteries were thickened, with more pronounced thickening on the right side than on the left side (Panel A). The arteries were also tender on palpation, with diminished pulses. The ophthalmic examination was normal. Laboratory studies showed an erythrocyte sedimentation rate (ESR) of 15 mm per hour (reference value, <14) and a C-reactive protein (CRP) level of 24 mg per liter (reference value, <10). Doppler ultrasonography of both temporal arteries revealed diffuse wall thickening with a “halo sign” — a hypoechoic area around the vessel lumen. Owing to concern about giant-cell arteritis, treatment with high-dose oral prednisolone was started. Biopsy of the right temporal artery revealed transmural thickening of the arterial wall with a lymphohistiocytic infiltrate and multinucleate giant cells (Panel B), which confirmed the diagnosis. In some cases of giant-cell arteritis, the ESR may not be markedly elevated, although it is uncommon for both the ESR and the CRP level to be normal. At the 1-week follow-up visit, the patient’s symptoms had abated, and a gradual tapering of the glucocorticoid dose was started at the 4-week follow-up visit.

