

Toxic Megacolon Due to Fulminant Clostridioides difficile Infection
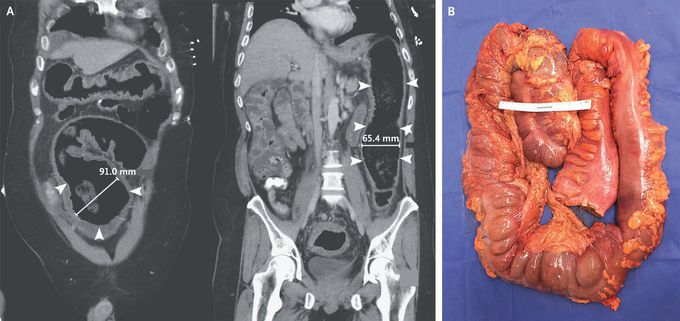
A 40-year-old man presented to the emergency department with vomiting and diarrhea. He had no known medical history and had not received antimicrobial therapy recently. His heart rate was 132 beats per minute, and other vital signs were normal. Examination was notable for confusion and for diffuse tenderness to palpation of the abdomen with tympany. Laboratory testing showed a white-cell count of 29,000 per cubic millimeter (reference range, 4000 to 10,800) and a positive nucleic acid amplification test for Clostridioides difficile. Computed tomography of the abdomen revealed pancolitis with distention of the sigmoid and descending colon (Panel A; arrowheads indicate the areas of distention, and two-dimensional measurements of colon width are shown). Despite 2 days of treatment with oral and rectal vancomycin and intravenous metronidazole, shock developed in the patient on hospital day 3. An urgently obtained radiograph of the abdomen showed worsening distention of the transverse colon near the hepatic flexure to 120 mm (abnormal width, >60 mm). Owing to concern for toxic megacolon due to fulminant C. difficile colitis, an emergency total colectomy with end ileostomy was performed. Gross pathological examination showed colonic dilatation with pseudomembranes (Panel B). Histopathological assessment showed pseudomembranous colitis, a finding consistent with C. difficile infection. The patient did well after surgery and was discharged 6 days after the procedure.
I was diagnosed as a Hepatitis B carrier in 2015, with early signs of liver fibrosis. At first, antiviral medications helped control the virus but over time, resistance developed, and the effectiveness faded. I began to lose hope. In 2021, I discovered NaturePath Herbal Clinic despite my skepticism, I decided to give their herbal treatment a try.To my surprise, after just six months, my blood tests came back negative for the virus.It was nothing short of life-changing.I never expected such incredible results from a natural treatment. But it not only cleared the virus it restored my hope, my health, and my peace of mind.If you or someone you know is battling Hepatitis B, I truly encourage you to explore the natural healing path offered by NaturePath Herbal Clinic. It gave me a second chance and it might do the same for you.www.naturepathherbalclinic.com info@naturepathherbalclinic.com


