

Occipital Calcification and Celiac Disease
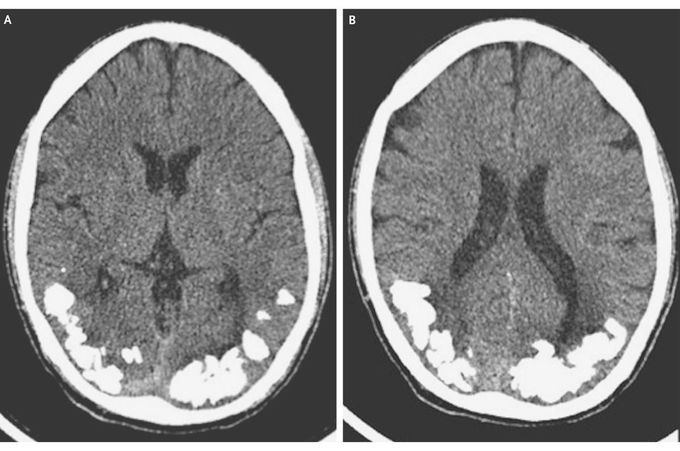
A 24-year-old man presented with a 10-year history of recurrent episodes of throbbing, occipital headache associated with complex visual symptoms, lasting from a few minutes to an hour. He had been treated for migraine, with little response. Routine blood tests revealed a mildly decreased folate level (2.2 ng per milliliter [5.0 nmol per liter]; reference range, 3.1 to 17.5 ng per milliliter [7.0 to 39.0 nmol per liter]), and a computed tomographic scan of the head revealed bilateral occipital calcification (Panels A and B). Laboratory testing revealed normal cerebrospinal fluid and elevated levels of serum IgA antitransglutaminase antibodies (45 U per milliliter; reference range, <10) and antiendomysial antibodies (titer, 1:40). He underwent endoscopy, and pathological evaluation of a jejunal-biopsy specimen revealed crypt hyperplasia, villous atrophy of the jejunal mucosa, and an increased number of intraepithelial lymphocytes. Treatment with a gluten-free diet, folic acid supplementation, and carbamazepine was initiated, and the patient's condition improved, with remission of all symptoms. The combination of celiac disease, epilepsy, and cerebral calcification is a rare condition known as the CEC syndrome. Folate malabsorption is a suggested mechanism, because cerebral calcification can be seen in other conditions related to folate deficiency, such as treatment with methotrexate, congenital folate malabsorption, and the Sturge–Weber syndrome.

