

Acute Neck Infection
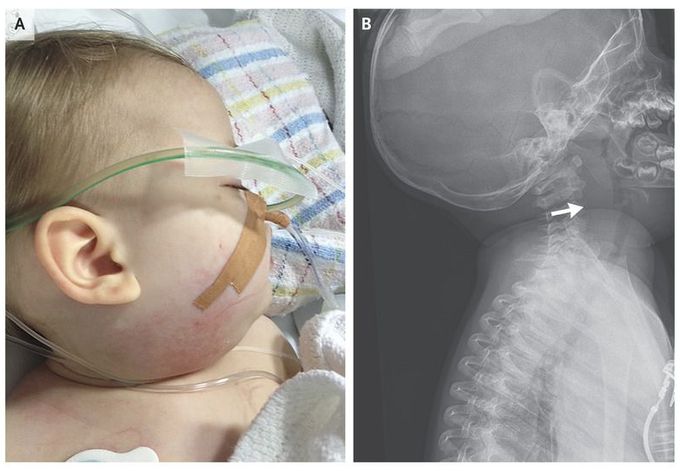
A fully immunized, previously well 11-month-old girl presented with a 4-day history of fever, coryza, and increasingly frequent respiratory grunting. On examination, she was febrile (temperature, 38.2°C), and had tachycardia and hypotension. She also had tachypnea, with mild stridor, and there was a fullness on the right side of her neck that developed on the day of presentation (Panel A). Lateral neck radiography revealed additional prevertebral swelling (Panel B, arrow), and an ultrasound scan showed multiple enlarged lymph nodes but no retropharyngeal abscess. The patient had neutropenia (5100 white cells per cubic millimeter and 2600 neutrophils per cubic millimeter) and an elevated level of C-reactive protein. She was treated with ceftriaxone, but her condition rapidly deteriorated, with progressive neck swelling, bilateral pleural effusions, and hepatosplenomegaly. Acidosis developed, and blood-product transfusions were required. The differential diagnosis included toxic shock syndrome, hemophagocytic lymphohistiocytosis, acute myeloid leukemia, lymphoma, and tumor lysis syndrome. Although blood cultures were negative, group A streptococcus grew on cultures of pleural fluid samples and a biopsy specimen from a cervical lymph node. The development of significant cervical lymphadenopathy concurrently with symptoms of shock appeared to be part of the initial group A streptococcal septic shock syndrome, with subsequent development of pleural effusions and organomegaly. The patient gradually improved, and antibiotics were ceased after 4 weeks, with complete resolution of lymphadenopathy and hepatosplenomegaly.

