

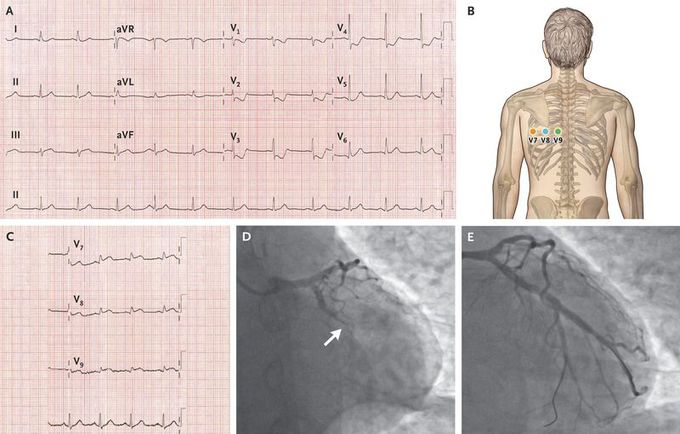
Posterior-Wall Myocardial Infarction
A 60-year-old woman who was a current smoker presented to the emergency department with acute chest pain. The troponin I level was 51 ng per liter on a high-sensitivity assay (reference value, <18 ng per liter). An electrocardiogram (ECG) showed sinus rhythm with ST-segment depressions in leads V1 through V4, with a positive terminal T wave and a large R wave in leads V2 and V3 (Panel A), an appearance suggestive of posterior-wall ischemia. An ECG performed with the use of posterior leads (Panel B) revealed ST-segment elevation in leads V7, V8, and V9 (Panel C). Emergency coronary angiography was performed. Occlusion of the proximal left circumflex coronary artery and the first obtuse marginal artery was visualized (Panel D, arrow) and treated with the placement of a drug-eluting stent (Panel E). Posterior-wall myocardial infarction can be challenging to diagnose because of the absence of ST-segment elevation on a standard 12-lead ECG. Posterior-lead placement is an important diagnostic tool if ischemia is suspected in the posterior wall. The patient’s subsequent clinical course was uneventful, and she was discharged while receiving medical therapy for secondary prevention. At the 3-month follow-up, the patient remained well.

