

Megaduodenum in Systemic Sclerosis
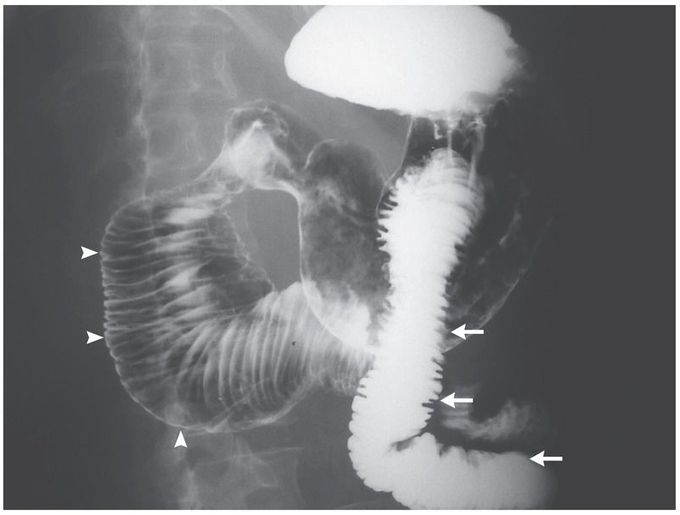
A 46-year-old woman who had a 7-year history of systemic sclerosis and used methotrexate for its treatment presented to the emergency department with abdominal pain, persistent nausea, and vomiting of undigested food that had begun 3 months earlier. On physical examination, she was noted to have skin with woody induration and loss of normal elasticity, dry eyes, and a decreased oral aperture. The physical examination of the abdomen was normal. Upper gastrointestinal endoscopy showed no evidence of mechanical obstruction or esophageal damage; a barium-swallow examination revealed duodenal distention of up to 8 cm in diameter (arrowheads), without evidence of mechanical obstruction, and normal intestinal caliber of the jejunum (arrows). Megaduodenum secondary to systemic sclerosis was diagnosed after assessments for other conditions, including amyloidosis, Chagas’ disease, and Whipple’s disease, were unrevealing. Assessments included biopsy of the distal duodenum and testing for antibodies to Trypanosoma cruzi and Tropheryma whipplei. Placement of a jejunostomy tube for feeding resulted in a reduction in the patient’s symptoms and a weight gain of nearly 4 kg over a period of 8 months. Gastrointestinal manifestations of systemic sclerosis may include esophageal and gastric dysmotility; duodenal involvement is rare.

