

Disseminated Varicella Infection
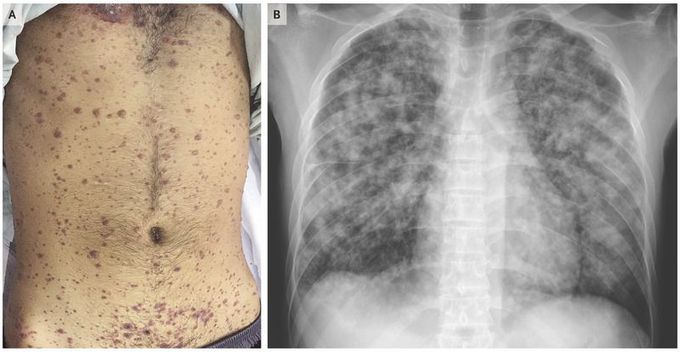
A 29-year-old man with a history of aplastic anemia who was being treated with cyclosporine presented to the emergency department with a 4-day history of fever, cough, and difficulty breathing at rest. One day before the onset of symptoms, a pruritic rash had developed on his face, trunk, and limbs. On physical examination, the pulse was 104 beats per minute, the blood pressure was 110/70 mm Hg, the respiratory rate was 36 breaths per minute, and the oxygen saturation was 90% while the patient was breathing high-flow oxygen. He had a diffuse rash at different stages of development, including papules, vesicles, pustules, and crusted vesicles (Panel A). Laboratory evaluation showed a platelet count of 33,000 per cubic millimeter (reference range, 150,000 to 400,000), an alanine aminotransferase level of 297 U per liter (reference range, 2 to 41), and an aspartate aminotransferase level of 281 U per liter (reference range, 2 to 40). A chest radiograph showed multiple nodules coalescing to form nodular consolidation and infiltrates in both lungs (Panel B). On the basis of his history of contact with a person who had chickenpox, along with the appearance of lesions and pulmonary symptoms in the context of immunosuppression, a clinical diagnosis of disseminated varicella infection was made. Despite treatment, which included intravenous acyclovir and mechanical ventilation with an acute respiratory distress syndrome protocol, the patient died 2 days after presentation.

