

Dubin–Johnson Syndrome
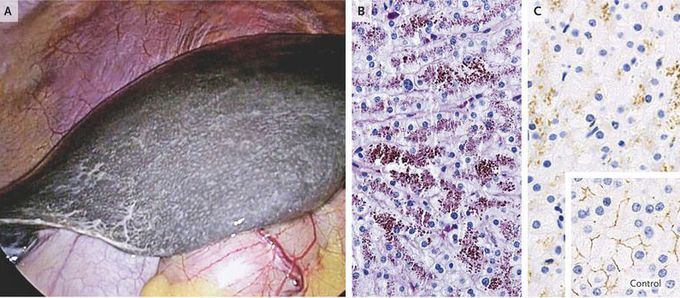
A 48-year-old woman scheduled to receive a laparoscopic cholecystectomy underwent a preoperative evaluation that disclosed conjugated hyperbilirubinemia. The serum total bilirubin level was 4.6 mg per deciliter (79 μmol per liter; reference range, 0.2 to 1.2 mg per liter [3 to 21 μmol per liter]), and the direct-reacting level was 2.4 mg per deciliter (41 μmol per liter; reference range, 0 to 0.3 mg per deciliter [0 to 5 μmol per liter]). The results of the physical examination, the prothrombin time and international normalized ratio, and serum levels of alanine aminotransferase and aspartate aminotransferase, alkaline phosphatase, and albumin were normal. The patient reported having had jaundice for decades, with no related symptoms. A laparoscopic exploration revealed a smooth liver with normal consistency and morphologic features but with a grossly black appearance (Panel A and video). A biopsy specimen revealed coarse, deep-brown, pigmented granules on periodic acid–Schiff staining (Panel B), primarily at the canalicular pole of the hepatocytes and especially in the pericentral zones, with otherwise well-preserved lobular architecture. Expression of the multidrug-resistance–associated protein 2 (MRP2) was absent on anti–MRP2 immunohistochemical analysis (Panel C; see also comparison with control specimen [inset]). A diagnosis of the Dubin–Johnson syndrome was confirmed. This syndrome is an autosomal recessive disorder that is caused by a mutation in MRP2 that results in deficient canalicular expression of MRP2 and impaired secretion of conjugated bilirubin into the bile. Such mutations cause an isolated increase in serum levels of conjugated bilirubin and the appearance of a black liver, without associated sequelae.

