

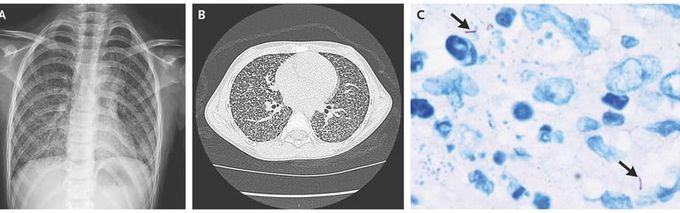
Drug-Resistant Miliary Tuberculosis in a Child
A previously healthy 8-year-old girl presented to the hospital with a 3-month history of dry cough and persistent fevers. A chest radiograph (Panel A) and a subsequent contrast-enhanced computed tomographic (CT) scan (Panel B) showed a diffuse, miliary (i.e., millet seed–like) pattern of uniformly sized, small nodules throughout both lungs. The soft-tissue window (not shown) revealed necrotic-appearing mediastinal lymph nodes. A tuberculin skin test and an interferon-γ release assay were positive, and a sputum acid-fast bacilli smear was negative. Cultures were obtained from multiple sources, including sputum, bronchoalveolar lavage, and cerebrospinal fluid. During the wait for the culture results, empirical first-line treatment for tuberculosis was initiated; however, the patient’s condition did not improve after 2 months of therapy. Because the cultures remained negative, a lung biopsy was performed with video-assisted thoracoscopy; a hematoxylin and eosin stain of the biopsy specimen showed caseous necrosis, and an acid-fast stain was positive for bacilli (Panel C, arrows). Drug-resistant tuberculosis was suspected. Because the results of tests to confirm drug resistance can take weeks to return, treatment was empirically changed to a regimen that is standard for drug-resistant tuberculosis in the region. The patient’s temperature returned to normal within 2 weeks after initiation of this treatment regimen, and repeat CT images at 2 months showed improvement. When the results of the drug-resistance tests were returned, isoniazid-resistant tuberculosis was confirmed.
What is the Tx regimen for isoniazid resistant tuberculosis Dr Sheikh? Assuming your practice is outside of the US, we don’t get to see rarities like this in US ERs or urgent cares.
This is my I WhatsApp number 9885937844 send hi I will send book

