

Xanthogranulomatous Pyelonephritis
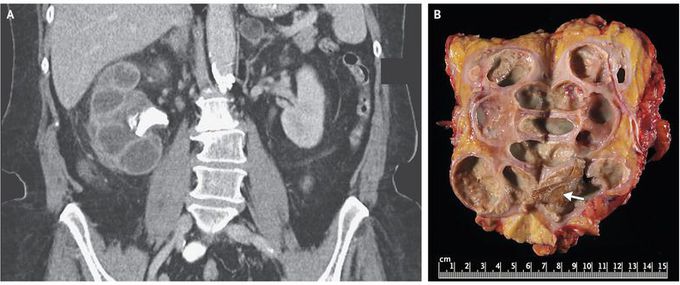
A 73-year-old woman presented to the emergency department with a 10-day history of fever and lethargy. Her medical history included type 2 diabetes, recurrent urinary tract infection, and weight loss of approximately 13.5 kg during the previous year. Laboratory studies revealed a white-cell count of 14,290 per cubic millimeter (reference range, 4500 to 11,000) and a serum creatinine level of 1.3 mg per deciliter (115 μmol per liter; reference range, 0.6 to 1.5 mg per deciliter [53 to 133 μmol per liter]); examination of the urine sediment revealed 50 to 100 white cells per high-powered field, but a culture was negative for bacteria. Computed tomography of the abdomen performed with the intravenous administration of contrast material (Panel A) revealed an enlarged right kidney with staghorn calculus in the ureteropelvic junction, cortical atrophy, and calyceal dilatation — an appearance referred to as a “bear paw sign.” Intravenous antibiotic agents were initiated, and percutaneous nephrostomy was performed. Culture of the drainage grew Proteus mirabilis. After a radionucleotide scan showed that renal function was absent on the right side, nephrectomy was performed. Gross pathological analysis showed a staghorn calculus (Panel B, arrow), dilated calyces, cystic cavities, and yellow tissue. Histologic testing revealed fibrosis and chronic granulomatous inflammatory infiltrate with lipid-laden foamy macrophages and necrotic debris. Xanthogranulomatous pyelonephritis was diagnosed. Xanthogranulomatous pyelonephritis, a form of chronic pyelonephritis, is typically associated with obstructing calculi and recurrent urinary tract infection. Complications may include abscesses and fistulae. Loss of renal function is common, and nephrectomy is the definitive treatment. The patient was discharged 5 days after surgery and was feeling well with stable renal function at 1 month of follow-up.

