

Tuberculous Pericarditis
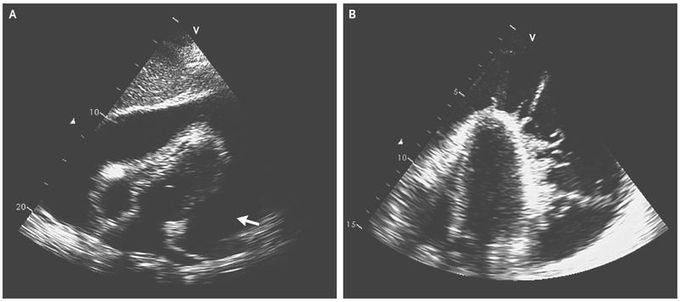
A 29-year-old woman presented to the emergency department with a 1-month history of worsening fatigue and weakness and a 2-week history of fever and dyspnea. She had emigrated from Angola 9 years before presentation. The temperature was 39.5°C, blood pressure 80/50 mm Hg, heart rate 135 beats per minute, and respiratory rate 32 breaths per minute. On examination, the patient’s neck veins were distended, and heart sounds were muffled. An electrocardiogram showed sinus tachycardia and low-voltage complexes in the limb and precordial leads. Transthoracic echocardiography revealed a large pericardial effusion with evidence of tamponade (Panel A [arrow]. The effusion contained extensive intrapericardial fibrin strands with a wormlike appearance . Pericardiocentesis was performed, and hemodynamic stability was achieved after direct aspiration of 1400 ml of purulent fluid; a pericardial drain was placed. The adenosine deaminase level in the pericardial fluid was 100 U per liter (reference range, 0 to 9), and examination of the pericardial fluid revealed acid-fast bacilli. A diagnosis of tuberculous pericarditis was made. Testing for human immunodeficiency virus was positive. The patient was treated with isoniazid, rifampin, pyrazinamide, and ethambutol for 2 months, followed by rifampin and isoniazid for an additional 4 months along with prednisolone for 6 weeks for prevention of constrictive pericarditis. Antiretroviral therapy was also initiated. The fevers resolved within the first week of treatment.

