

Lymphangioleiomyomatosis
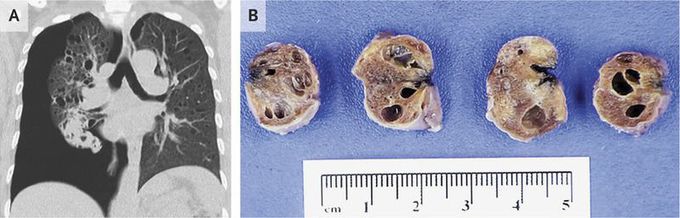
A 44-year-old woman presented to the emergency department with acute chest pain after several months of progressive dyspnea. Her oxygen saturation was 92% while she was breathing ambient air, and the physical examination was notable for diminished breath sounds on the right side. Computed tomography of the chest, reconstructed in the coronal plane at the level of the tracheal carina, revealed a large pneumothorax and diffuse, intraparenchymal pulmonary cysts (Panel A). The patient underwent mechanical pleurodesis, and a wedge biopsy was performed. The biopsy specimens contained numerous thin-walled cysts (Panel B). Spindle cells coexpressing smooth-muscle and melanocytic markers lined the cyst walls, which confirmed the diagnosis of lymphangioleiomyomatosis, a rare condition that can affect women of all ages, with the average age at diagnosis in the late 30s to early 40s. Symptoms may occur sporadically or in association with tuberous sclerosis complex. Activation of the mechanistic (formerly mammalian) target of rapamycin (mTOR) signaling pathway causes aberrant cell proliferation and lymphangiogenesis. Several weeks after the patient’s presentation, recurrent sharp chest pain and dyspnea developed. Chest radiography revealed a contralateral spontaneous pneumothorax resulting from cyst rupture. After pleurodesis, her dyspnea persisted, and pulmonary-function testing revealed a forced expiratory volume in 1 second (FEV1) that was 44% of the predicted value. Within 3 months after the initiation of therapy with sirolimus, an mTOR inhibitor, her exercise tolerance had improved (with an FEV1 that was 67% of the predicted value), but she continued to have fatigue and chest discomfort and had not returned to work.

