

Esophageal Atresia and Tracheoesophageal Fistula
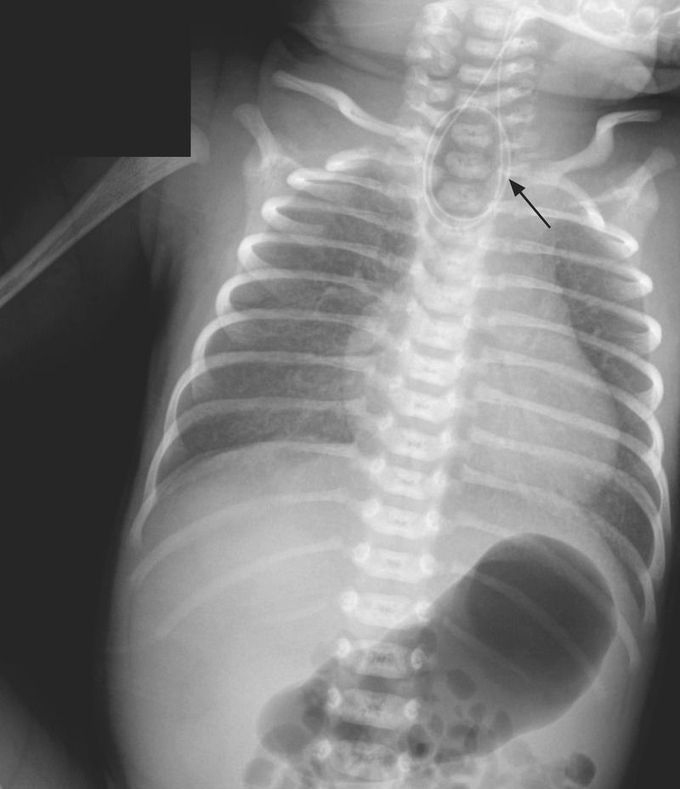
An infant had an apneic episode at birth and received positive-pressure ventilation in the delivery room during neonatal resuscitation. The infant had a birth weight of 2400 g (5th percentile) and was born to a 39-year-old woman who had presented for a planned cesarean section at 37 weeks 2 days of gestation. The prenatal course had been complicated by obesity, poorly controlled gestational diabetes, and polyhydramnios. Prenatal ultrasonography had not revealed fetal abnormalities. The Apgar scores were 1 point at 1 minute and 9 points at 5 minutes. Owing to the infant’s copious oral secretions, a nasogastric tube was inserted but met resistance at 11 cm. A chest radiograph showed the catheter coiled in the esophagus (arrow) at the level of the second thoracic vertebra and air in the stomach. Esophageal atresia with tracheoesophageal fistula, type C, was diagnosed. Type C, the most common type, is characterized by a proximal esophageal pouch with a distal tracheoesophageal fistula. Esophageal atresia and tracheoesophageal fistula may be associated with congenital vertebral, anorectal, cardiovascular, renal, and limb defects (collectively known as the VACTERL association). Physical examination, echocardiography, and renal ultrasonography did not reveal associated abnormalities. Primary esophagoesophagostomy and ligation of the tracheoesophageal fistula were performed on day 2. The patient began feeding by mouth on day 9 and was discharged on day 33. At follow-up visits at 2, 4, and 6 months of age, the infant was growing and developing well.

