

Arrhythmia
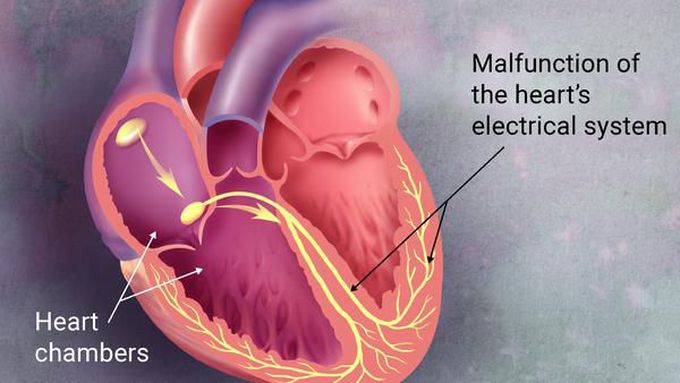
Antidysrhythmic medications are widely used to treat or prevent abnormalities in cardiac rhythms. They accomplish this through a number of mechanisms involving automaticity or ion channel dynamics, which in turn affect the propagation of the myocardial electrical impulse via change in conduction velocity or refractory period. Antidysrhythmics alter the propagation and mechanisms of cardiac rhythms, making toxicity from these agents highly lethal. In fact, antidysrythmics can be prodysrhythmic at both therapeutic and toxic serum concentrations. Additionally, the patients receiving these drugs may have a lower dysrhythmic threshold resulting from underlying cardiac conditions as well as other comorbidities, making them more suscpetible to toxicity. A thorough knowledge of this class of drugs is necessary for differentiating drug toxicity from primary disease. Signs and symptoms Toxicity from antidysrhythmic agents can be grouped in terms of clinical presentation and electrocardiographic (ECG) abnormalities, as follows: Anticholinergic syndromes: Procainamide, disopyramide, quinidine Heart failure: Disopyramide, flecainide, propafenone, sotalol, procainamide Hypotension: Quinidine, procainamide, amiodarone, dronedarone, lidocaine, mexiletine, flecainide, propafenone, ibutilide CNS symptoms: Quinidine, procainamide, disopyramide, lidocaine, mexiletine, flecainide, propafenone Seizures (acute toxicity): Quinidine, procainamide, lidocaine, mexiletine, flecainide, propafenone Endocrine dysfunction: Amiodarone (hypothyroidism or hyperthyroidism), quinidine and disopyramide (hypoglycemia) Hematology/Oncology: Amiodarone (hepatic/biliary malignancy), procainamide (blood dyscrasia) Pulmonary/autoimmune: Procainamide (lupuslike syndrome, vasculitis), amiodorone (fibrosis, pneumonitis) CNS: procainamide, lidocaine, mexilitine Dermatologic: procainamide, propafenone ECG changes are as follows: QRS widening: Quinidine, procainamide, disopyramide, flecainide, propafenone, amiodarone, dronedarone PR prolongation: procainamide QTc prolongation: Quinidine, procainamide, disopyramide, amiodarone, dronedarone, sotalol, ibutilide, dofetilide; slight prolongation with flecainide, propafenone Ventricular arrythmia (ventricular premature contractions or ventricular tachycardia): Procainamide Torsade de pointes: Ibutilide, dofetilide, sotalol, quinidine, procainamide, disopyramide Diagnosis The first and most important diagnostic tool in acute antidysrhythmic toxicity is electrocardiography. ECG changes such as QRS widening, QTc prolongation, and atrioventricular block should be ruled out. Serum electrolytes concentrations should be obtained, especially in patients taking antidysrhythmics that prolong the correct QT (QTc) interval. Serum drug concentrations are not likely to be helpful to the emergency physician treating a patient with acute antidysrhythmic drug toxicity, but concentrations of quinidine, lidocaine, and propafenone can be measured in the acute care setting. Chest radiographs and brain natriuretic peptide levels should be obtained in patients presenting with heart failure symptoms; Chest radiographs should also be obtained in patients taking amiodarone or dronedarone and presenting with pulmonary symptoms. Thyroid function tests should be obtained in patients taking amiodarone or dronedarone who present with signs and symptoms of hypothyroidism or hyperthyroidism. Management Airway, breathing, and circulatory support; intravenous access; and ECG monitoring are of paramount importance. Treatment measures and the drugs for which they are appropriate are as follows: GI decontamination: Should be considered in most antidyrthymmic overdose, and specifically with disopyramide, quinidine, flecainide, propafenone, amiodarone Hemodialysis: Procainamide, mexiletine, sotalol Sodium bicarbonate: Class Ia and Ic antidysrhythmics (quinidine, procainamide, disopyramide, lidocaine, mexiletine, flecainide, propafenone) Magnesium: Class III agents, Ibutilide, dofetilide, sotalol, quinidine, procainamide, disopyramide Intravenous lipid emulsion: Verapamil; less evidence for lidocaine, flecainide, amiodarone Seizure control (benzodiazepines): Quinidine, procainamide, lidocaine, mexiletine, flecainide, propafenone Background Despite the advent of interventional techniques such as catheter ablation and the implantable cardioverter-defibrillator in the treatment of supraventricular and ventricular tachycardia, antidysrhythmic drugs continue to play a significant role in treating and suppressing life-threatening dysrhythmias. The prodysrhythmic effects of many of these drugs also continue to present a major clinical problem, especially in the growing population of patients with underlying heart failure. When encountering a patient with dysrhythmias on antidysythmic drugs, the physician must maintain a broad differential diagnosis that includes not only drug toxicity but underlying ischemia, structural cardiac abnormalities, and conduction disturbances. Thus, understanding the adverse effects and electrocardiographic profiles of antidysrhythmic agents is critical for diagnosis and treatment of possibly life-threatening drug toxicity. This article discusses the major antidysrhythmic drugs within classes I, III and V, with specific attention to their adverse effects and clinical presentations in the setting of acute toxicity. Toxicity from class II and IV dysrhythmics is discussed elsewhere (see Beta-Blocker Toxicity and Calcium Channel Blocker Toxicity) For additional information, see Medscape's Cardiology Resource Center. For patient education resources, see the First Aid and Injuries Center, as well as Poisoning, Drug Overdose, Activated Charcoal, and Poison Proofing Your Home. Pathophysiology Most antidysrythmics may be categorized via the Vaughan-Williams classification system, based on their mechanism of activity (see the image below). Medications used to treat arrhythmias that have variable mechanisms have been included in class V; these include magnesium, digoxin, and adenosine. The Vaughn-Williams classes are as follows: Class I: Sodium channel blockers Class II: Beta-adrenergic blockers Class III: Potassium channel blockers Class IV: Calcium channel blockers Class V: Other or unknown mechanism of action
Living with Pulmonary Fibrosis (PF) was one of the hardest experiences of my life. The breathlessness, the fatigue, and the fear of the future weighed on me every single day. I had tried so many treatments and medications, but nothing seemed to stop the disease from progressing.Out of both hope and desperation, I came across NaturePath Herbal Clinic. At first, I was skeptical but something about their natural approach and the stories I read gave me the courage to try one more time.I began their herbal treatment program, and within a few weeks, I noticed small changes easier breathing, more energy, and a clearer mind. Over themonths, those improvements became more and more obvious. Today, I can truly say my life has changed. My lungs feel stronger, and my quality of life has returned in ways I didn’t think were possible.This isn’t just a testimony it’s a heartfelt recommendation to anyone struggling with PF or other chronic conditions. Don’t give up hope. I’m so grateful I gave NaturePath Herbal Clinic a chance. Visit their website to learn more: www.naturepathherbalclinic.com info@naturepathherbalclinic.com



