

Radial Keratotomy
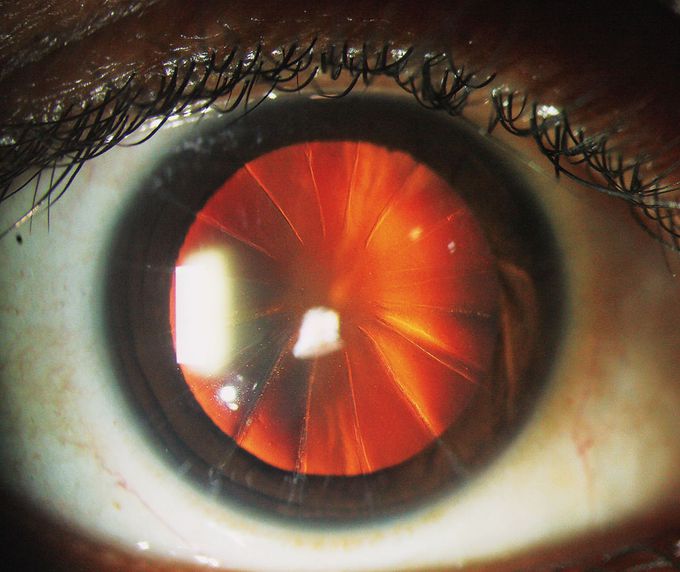
A 41-year-old woman presented to the ophthalmology clinic with vision that had been deteriorating during the preceding 20 years. Her subjective refraction showed that a hyperopic shift had occurred since her current corrective lenses had been prescribed. Her best corrected visual acuity was 20/25 in both eyes. Slit-lamp examination revealed features that suggested that radial keratotomy had been performed: a clear central cornea with 16 corneal incisions extending from the periphery. Because radial keratotomies are performed manually, the incisions are neither perfectly radial nor symmetric. The patient confirmed that she had undergone this surgery for the treatment of myopia 23 years before presentation. At the time of the procedure, she had had no immediate complications. Radial keratotomy was frequently performed in the 1980s and 1990s to correct myopic refractive errors. However, the procedure is associated with a number of complications. Overlapping or excessively central incisions may lead to reduced visual acuity, and corneal scarring is associated with glare and halos. Patients are at risk for progressive hyperopia and, in rare cases, owing to reduced corneal biomechanical strength, globe rupture with minimal trauma. The patient received a new prescription for corrective lenses and was advised of the importance of protective eyewear. At a 6-month follow-up visit, her vision had not deteriorated further. Sahib Y. Tuteja, B.Sc. Manchester Medical School, Manchester, United Kingdom Muralidhar Ramappa, M.D. LV Prasad Eye Institute, Hyderabad, India source: nejm.org
Acute Conjunctivitis (Pink Eye) | Allergic, Bacterial, Viral | Symptoms, Diagnosis, TreatmentWhat causes eye freckles? Are they dangerous?Strabismus: Everything You Need To KnowFATTY DEPOSITS of CHOLESTEROL around EYES | How to get rid of it?-Dr.Rajdeep Mysore|Doctors' CircleGlaucomaApical cystectomyMandibular deviation following Hemimandibulectomy

