

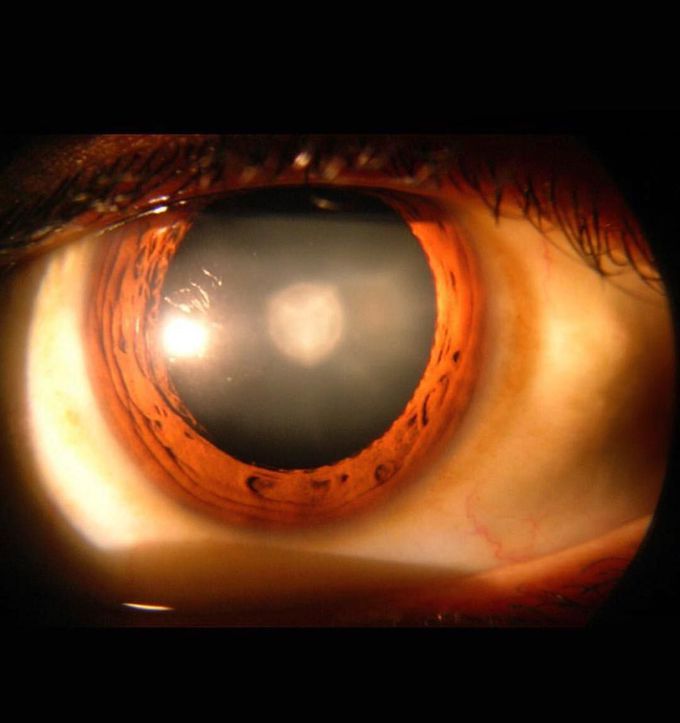
THE POSTERIOR POLAR CATARACT
This is a very rare type of cataract called “THE POSTERIOR POLAR CATARACT”. A posterior polar cataract is a round, discoid, opaque mass (as in the above image) that is composed of malformed and distorted lens fibers located in the central posterior part of the lens.This location is its most significant feature, in addition to its proximity to and possible adherence with the posterior capsule. The human lens is composed of proteins arranged in a specific way to keep it clear and allow light to pass through. It then focuses all the light to the retina, which then sends signals to the fovea centralis (in the macula lutea) and optic nerve to produce vision. As we age, however, it is believed that those proteins clump together, causing a "cloud" to form. When the lens becomes opaque, or cloudy/foggy, most of its refractory properties are lost and light has a difficult time getting through. This adulterates the signals sent to the receptors, resulting in vision described as if looking through a steamy mirror or foggy window. Most cataracts are slow and due to aging. It can also be formed by disease such as diabetes, smoking/alcohol use, and prolonged exposure to UV sunlight. •Signs and sumptoms: Common signs and symptoms include cloudy/blurry vision, complaint of faded colors, double vision in one or both eyes, poor night vision. A halo around the pupil may also be found upon physical examination. •Treatment: Treatments most often include lens replacement. During cataract surgery, the cloudy lens is removed or cleaned out and replaced by a clear man made lens. Most cataract surgeries are done with a technique called phacoemulsification, also called "small cut cataract surgery."
Posterior polar cataract is attached to the posterior capsule. To be able to leave the capsule intact requires a skilled surgeon. Capsulorexhis on the anterior capsule is performed, lenticular fibers are phacoemsified then a second capsulorexhis is performed to remove the ppc essentially leaving the capsule bag in a tire form. So both ends will have an opening. Then the new IOL (intraocular lens) is placed in the “tire”. This is especially difficult to do because of the thinness of the capsular tissue, zonular adherence, and ability to inject the IOL between the capsules without dropping it on the macula. Average ophthalmologist will place three IOL in the sulcus; Not a bad option, still a good outcome.

