

Intravascular Large B-Cell Lymphoma
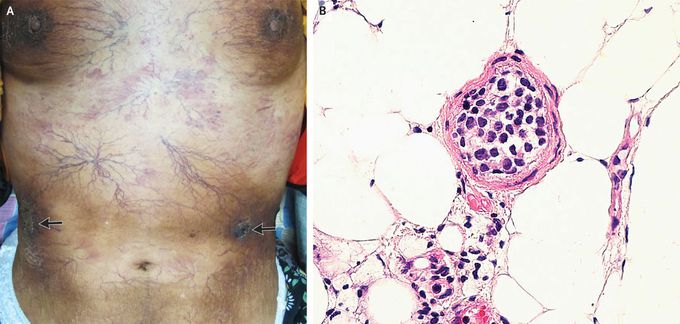
A 53-year-old woman presented to the dermatology clinic with a 3-month history of worsening vascular skin lesions and a 1-month history of fever. On physical examination, diffuse telangiectasias, hyperpigmented plaques, and several ulcerated nodules (arrows) were observed on the skin across the chest and abdomen (Panel A) and the legs. No palpable lymphadenopathy or hepatosplenomegaly was noted. Laboratory studies were notable for a lactate dehydrogenase level of 356 U per liter (reference range, 120 to 250). A deep skin-biopsy specimen from the abdomen showed intravascular aggregation of round, atypical lymphocytes (Panel B, hematoxylin and eosin staining). Subsequent immunohistochemical staining was positive for CD20, PAX-5, and MUM-1 in the neoplastic cells. A positron-emission tomographic–computed tomographic scan was negative. A diagnosis of intravascular large B-cell lymphoma was made. Intravascular large B-cell lymphoma is a rare, often aggressive extranodal lymphoma characterized by malignant involvement within the lumens of small vessels. The disease is challenging to diagnose owing to its nonspecific symptoms and signs (e.g., fever, fatigue, and absence of lymphadenopathy) and heterogeneous presentation. In this case, the patient’s isolated skin involvement was consistent with the cutaneous subtype of intravascular large B-cell lymphoma. Treatment with systemic chemotherapy was initiated. At the 6-month follow-up visit, the patient continued to be in remission.

