

Scleromyxedema
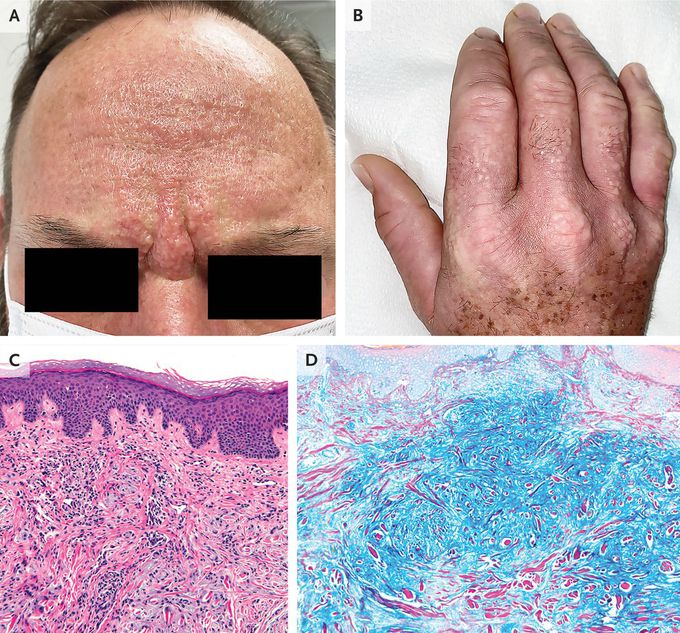
A 53-year-old man presented to the rheumatology clinic with a 3-year history of an itchy rash, Raynaud’s phenomenon, dysphagia, and a burning sensation in his hands. Physical examination was notable for firm, greasy papules across his forehead that led to the formation of glabellar grooves (Panel A). There were waxy papules on his hands, with associated skin thickening and finger flexion contractures (Panel B). Similar skin changes were seen on his nose, lips, ears, trunk, and feet. There was no telangiectasia or calcinosis. Sensory neuropathy was present in his hands, arms, and face. Tests of thyroid function were normal. Serum protein electrophoresis with immunofixation identified an IgG-λ monoclonal gammopathy, and a bone marrow biopsy was normal. A subsequent skin-biopsy sample obtained from the right side of the neck showed dermal spindle-cell proliferation, thickened collagen fibers, fibrosis, and perivascular inflammation (Panel C, hematoxylin and eosin stain), as well as increased dermal mucin deposition (Panel D, colloidal iron stain). A diagnosis of scleromyxedema was made. Scleromyxedema is a primary cutaneous mucinosis typically associated with a paraproteinemia. This type of sclerosing skin disorder may cause extracutaneous symptoms, as was seen in this patient. Although infusions of intravenous immune globulin provided minimal relief initially, treatment with lenalidomide resulted in abatement of symptoms and reduction in paraproteinemia after 4 months.


