

Terson’s Syndrome
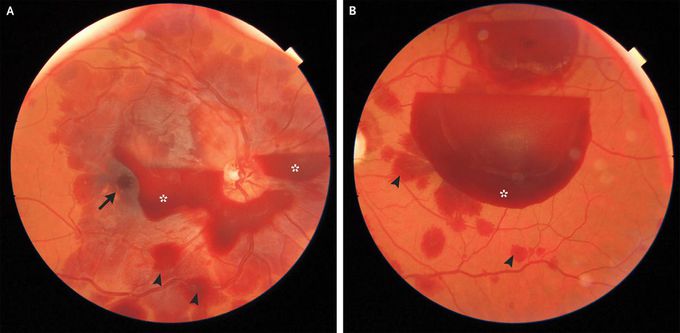
A 41-year-old man presented to the emergency department with a 2-day history of blurred vision and throbbing headache associated with nausea and vomiting. He had a history of hypertension, tobacco use, and a subarachnoid hemorrhage that had occurred 10 years earlier; the hemorrhage had been caused by an aneurysm of the anterior communicating artery on the right side for which he had subsequently undergone coil embolization. At the current presentation, his blood pressure was 147/93 mm Hg. A neurologic examination was normal. Visual acuity was 20/400 in the right eye and was limited to finger counting in the left eye. A nondilated funduscopic examination revealed preretinal hemorrhages in both eyes (Panels A and B [right and left eye, respectively], asterisks). A subretinal hemorrhage in the right eye (arrow) and intraretinal hemorrhages in both eyes (arrowheads) were also seen. The patient’s medical history and the finding of vitreous hemorrhages in both eyes suggested the possibility of Terson’s syndrome, which is characterized by the presence of multilayered intraocular hemorrhages in combination with subarachnoid hemorrhages. Computed tomography of the head identified a subarachnoid hemorrhage on the left side. Cerebral angiography was subsequently performed; a dissection of a left middle cerebral artery aneurysm was identified, and a stent was placed. At a 4-month follow-up visit, the patient’s visual acuity had improved to 20/100 in the right eye and to 20/60 in the left eye. Mild vitreous and subretinal hemorrhages persisted in both eyes.

