

Pulmonary Langerhans-Cell Histiocytosis
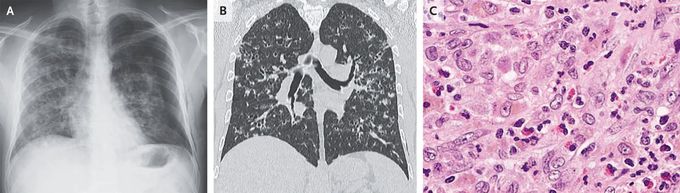
A 40-year-old man with a history of smoking presented to the emergency department with a 2-week history of cough, dyspnea, night sweats, and pleuritic chest pain on the left side. Physical examination was notable for decreased breath sounds over the left lung fields. A chest radiograph showed a large pneumothorax on the left side and interstitial infiltrates in both lungs (Panel A). The pneumothorax was treated with chest-tube thoracostomy. Subsequent computed tomography of the chest showed multiple cysts and nodules, predominantly in the upper and middle lung fields, with sparing of the costophrenic angles (Panel B). A transbronchial lung biopsy was performed. Histopathological tests showed a lymphocytic lung infiltrate with interalveolar septal thickening, eosinophils, and large cells with foamy cytoplasm and large nuclei (Panel C). Immunohistochemical staining was positive for S-100 protein, CD1a, placental acid phosphatase, and langerin. A diagnosis of pulmonary Langerhans-cell histiocytosis was made. Further testing revealed no evidence of systemic histiocytosis. BRAF testing was not done. The patient was advised to stop smoking, and a tapering dose of prednisone was prescribed. At the 6-month follow-up, the patient had ceased smoking; he was still taking low-dose prednisone, and his symptoms had abated.

