

Malignant Syphilis
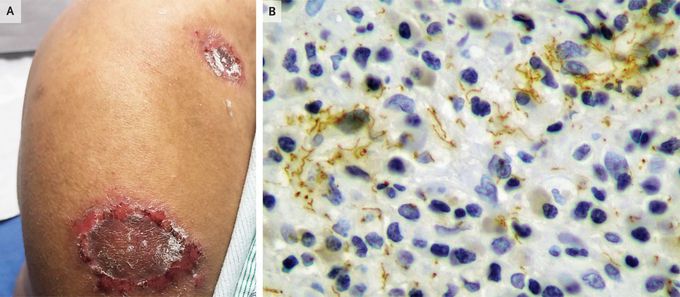
A 42-year-old man with human immunodeficiency virus (HIV) infection presented to the infectious disease clinic with a 1-month history of painful skin ulcerations associated with fevers, chills, weight loss, and headache. He had not been receiving HIV antiretroviral therapy owing to difficulties with clinic follow-up visits on account of his social circumstances. Physical examination revealed large ulcers with overlying keratosis and crusting scattered across his scalp, face, perineum, and limbs (Panel A, right shoulder). Findings from laboratory studies were notable for a CD4 count of 399 cells per cubic millimeter (reference range, 397 to 1719), a viral load of 102,000 copies per milliliter (reference value, <20), and an elevated rapid plasma reagin titer of 1:512. The patient declined a lumbar puncture to evaluate for neurosyphilis. A skin-biopsy sample showed superficial dermal infiltration of lymphocytes, histiocytes, and plasma cells in a poorly formed lichenoid pattern with overlying psoriasiform epidermal hyperplasia, and immunohistochemical analysis revealed the presence of spirochetes (Panel B, spirochete immunostain). The patient received a diagnosis of malignant syphilis, an uncommon form of secondary syphilis characterized by systemic symptoms and a papulopustular eruption that evolves into painful, necrotic ulcers. He also received a diagnosis of possible neurosyphilis. The patient’s symptoms were reduced with the administration of intravenous penicillin G, but he was later lost to follow-up.
Living with HIV was one of the hardest experiences of my life. The fatigue, the emotional toll, and the uncertainty about the future weighed on me every single day. I had tried many treatments and medications, but nothing seemed to restore my health or energy the way I hoped.Out of both hope and desperation, I came across NaturePath Herbal Clinic. At first, I was skeptical but something about their natural approach and the powerful stories I read gave me the courage to try one more time.I began their herbal treatment program, and within a few weeks, I noticed small but meaningful changes more energy, better sleep, and a stronger immune system. Over the months, those improvements only grew. Today, I can truly say my life has changed. I feel healthier, more balanced, and finally in control of my well-being again.This isn’t just a testimony it’s a heartfelt recommendation to anyone living with HIV or any chronic condition. Don’t give up hope. I’m so grateful I gave NaturePath Herbal Clinic a chance. Visit their website to learn more: www.naturepathherbalclinic.com Email: info@naturepathherbalclinic.com


