

Blastic Plasmacytoid Dendritic-Cell Neoplasm
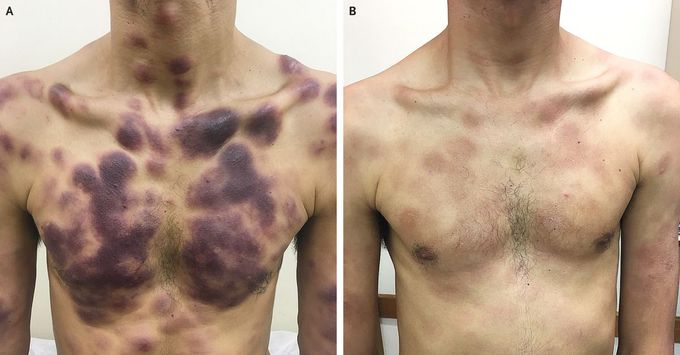
A 29-year-old man was referred to the hematology clinic with a 6-month history of progressive painless, nonpruritic skin lesions. He had no systemic symptoms, such as night sweats or weight loss. The physical examination showed extensive violaceous lesions on the face, back, trunk, and limbs (Panel A). Skin biopsy showed diffuse dermal infiltrate with blast-like cells extending to the hypodermis. Immunohistochemical analysis showed cells that were positive for CD4, CD56, and CD123, which supported the diagnosis of blastic plasmacytoid dendritic-cell neoplasm, a rare hematologic cancer. Computed tomographic scans did not reveal evidence of extracutaneous disease. Bone marrow aspiration showed the presence of 1% neoplastic plasmacytoid dendritic cells. The patient received a 1-week course of dexamethasone and had a substantial reduction in the cutaneous lesions (Panel B). He was then treated with eight cycles of hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, and dexamethasone) alternating with high-dose methotrexate and cytarabine, a course of therapy that resulted in complete remission. Blastic plasmacytoid dendritic-cell neoplasm is a systemic disease, although it can manifest with cutaneous lesions. It is important to obtain complete staging evaluation before the initiation of therapy, including the use of glucocorticoids. After the patient was clinically free from disease for 6 months, the disease relapsed, and the patient did not have a response to further treatment. He died 27 months after the diagnosis.

