

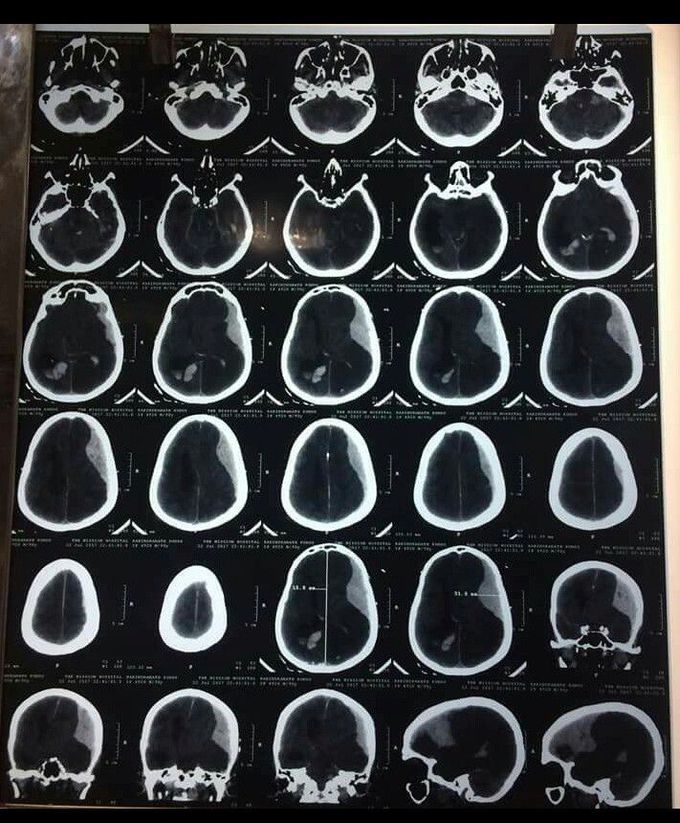
A patient presents to you in ER, after a road traffic accident. You get a brain CT scan done. It shows these findings. What is your diagnosis?
ACUTE SUBDURAL HEMATOMA is the result of an accumulation of blood between the arachnoid membrane and the dura. It usually results from venous bleeding, typically from tearing of a bridging vein running from the cerebral cortex to the dural sinuses. The bridging veins are subject to stretching and tearing during acceleration/deceleration of the head because the brain shifts in relation to the dura, which firmly adheres to the skull. Elderly and alcoholic patients are at higher risk for acute SDH formation after head trauma due to brain atrophy. head CT scan: the clot is bright or mixed-density, crescent-shaped (lunate), may have a less distinct border, and does not cross the midline due to the presence of the falx. Most SDHs occur over the cerebral hemispheres, but they may also occur between the hemispheres or layer over the tentorium. Open craniotomy for evacuation of acute SDH is indicated for any of the following: thickness >1 cm, midline shift >5 mm, or GCS drop by two or more points from the time of injury to hospitalization. Nonoperatively managed hematomas may stabilize and eventually reabsorb, or evolve into chronic SDHs. This management requires frequent neurologic examinations until the clot stabilizes based on serial head CT scans. Prognosis for functional recovery is significantly worse for acute SDH than EDH because it is associated with greater primary injury to brain parenchyma from high-energy impacts. Prompt recognition and intervention minimizes secondary injury. The elderly patients with low admission GCS, or high postoperative ICP do poorly, with as few as 5% attaining functional recovery. Source: Schawrt’z Principles of Surgery

