

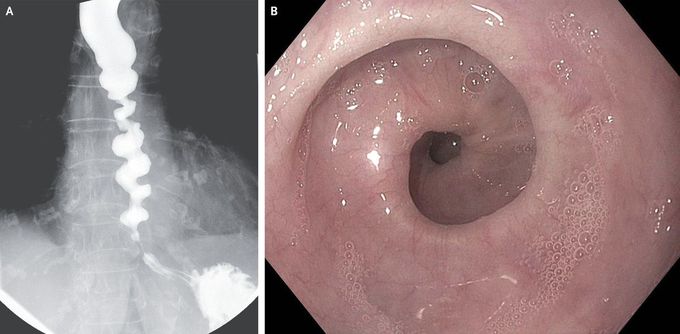
Corkscrew Esophagus in Achalasia
An 83-year-old woman presented to the gastroenterology clinic with dysphagia and regurgitation that occurred with every meal in association with postprandial chest pain. For several years, she had had difficulty swallowing both solids and liquids, and this symptom had worsened during the year before presentation. She also reported a weight loss of 9 kg in the previous year. A barium esophagram showed a corkscrew pattern (Panel A). Upper endoscopy was notable for nonperistaltic spastic contractions (Panel B) and a tight gastroesophageal junction. High-resolution esophageal manometry showed an elevated integrated relaxation pressure of the lower esophageal sphincter, absence of peristalsis, and spastic contractions consistent with type III (spastic) achalasia. The patient declined endoscopic myotomy and opted for treatment with endoscopic injection of botulinum toxin. At follow-up 5 months after treatment, she had only intermittent dysphagia and no regurgitation.

