

Advanced Mycosis Fungoides
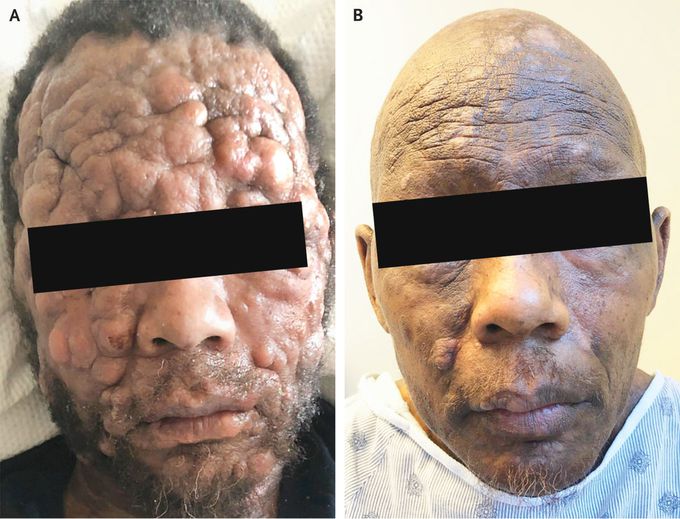
A 53-year-old man with a history of treated stage 1A mycosis fungoides that had been diagnosed 7 years earlier presented with a 2-month history of new and rapidly progressing lesions on his face and body. Examination of the head and neck showed multiple coalescing subcutaneous nodular lesions and deep furrowing of skin folds that resulted in distortion of the patient’s facial features (Panel A). Also present were numerous hyperpigmented erythematous nodules, as well as crusted hyperkeratotic tumors affecting approximately 85% of the patient’s total body-surface area. Flow cytometry of the peripheral blood identified a small population of atypical lymphocytes, and positron-emission tomography showed increased fluorodeoxyglucose uptake in the cervical, axillary, and pelvic lymph nodes, as well as in the spleen and liver. A skin biopsy confirmed the diagnosis of mycosis fungoides with CD30-expressing large-cell transformation. The patient began a regimen of brentuximab, cyclophosphamide, doxorubicin, and prednisone, and notable improvement was seen after two cycles (Panel B).



