

Hepatopulmonary Syndrome
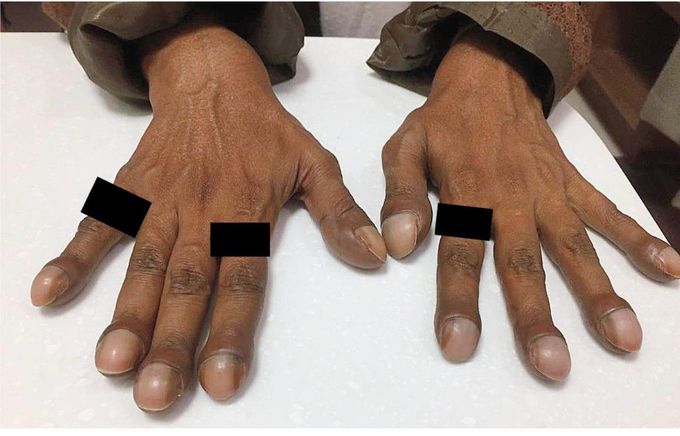
A 50-year-old man with cryptogenic cirrhosis presented to the gastroenterology clinic with a 2-year history of progressive shortness of breath on exertion. Findings on physical examination included ascites and pedal edema, splenomegaly, spider nevi, and finger clubbing. No abnormal sounds were heard on lung and heart auscultation. While breathing ambient air, the patient had an oxygen saturation, as measured by pulse oximetry, of 94% when in the supine position and of 88% when in an upright position. Arterial blood gas analysis, performed with the patient breathing ambient air while seated, showed a partial pressure of arterial oxygen of 60 mm Hg with an alveolar–arterial oxygen gradient of 54 mm Hg. Transthoracic echocardiography with intravenous agitated saline revealed opacification of the chambers on the left side of the heart by microbubbles five heartbeats after the appearance of microbubbles in the right atrium (see video), a finding suggestive of abnormal intrapulmonary vascular dilatations leading to intrapulmonary shunting. These findings were consistent with a diagnosis of hepatopulmonary syndrome. Medical management of cirrhosis in the patient, which included the use of diuretics, was initiated. At the 4-month follow-up, the patient had persistent shortness of breath.
Video link. https://youtu.be/gPnl1LX91vw


