

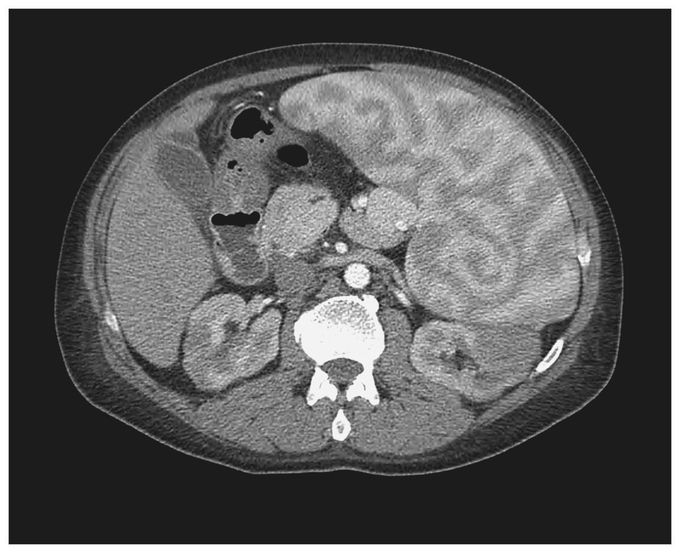
Enlarged Spleen with a Heterogeneous Pattern
A 50-year-old man with a history of warm-antibody autoimmune hemolytic anemia and splenomegaly presented with fatigue of 2 weeks' duration and the recent onset of jaundice. Physical examination revealed scleral icterus, conjunctival pallor, and splenomegaly. Laboratory tests revealed a hemoglobin level of 4.8 g per deciliter, a hematocrit of 14.3%, a white-cell count of 3200 per cubic millimeter, and a platelet count of 42,000 per cubic millimeter. Treatment with prednisone and intravenous immune globulin was initiated, and the patient underwent transfusion with multiple units of packed red cells during his hospital stay. Computed tomography of the abdomen with the use of nonionic contrast material revealed an enlarged spleen (25.4 cm craniocaudally, 18.1 cm anteroposteriorly, and 22.5 cm transversely) with a heterogeneous pattern. This pattern was seen during the initial 60 seconds after the injection of contrast material. It has previously been described as a series of alternating bands of high and low attenuation due to variability in blood flow between the red and white pulp of the spleen. The prominence of the heterogeneous pattern in this spleen is due to splenomegaly. The patient subsequently underwent splenectomy; a small monoclonal B-cell population was identified by means of flow cytometry. The patient's leukopenia and thrombocytopenia resolved (white-cell count, 10,500 per cubic millimeter; platelet count, 178,000 per cubic millimeter), and the hemoglobin level stabilized at more than 10.0 g per deciliter.

