

Crazy Paving in Pulmonary Alveolar Proteinosis
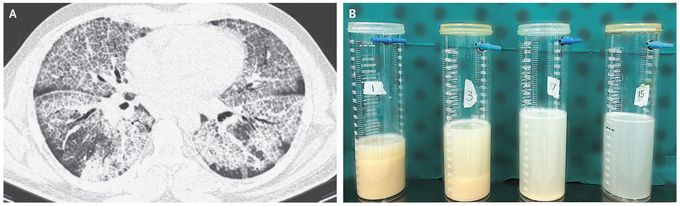
A 34-year-old man with a 20-pack-year smoking history presented to the emergency department with a 4-month history of progressively worsening dyspnea and nonproductive cough. The oxygen saturation was 65% while the patient was breathing ambient air. He appeared to have dyspnea at rest, his fingers and lips were blue, and his fingers showed clubbing. Sounds on auscultation of the lungs were normal. Computed tomography of the chest revealed diffuse ground-glass opacities with interlobular and intralobular septal thickening — a pattern described as crazy paving (Panel A). Bronchoscopy yielded milky-appearing lavage fluid, and pathological testing showed macrophages filled with proteinaceous material that was positive on periodic acid–Schiff staining, as well as large acellular eosinophilic aggregates. These findings confirmed a diagnosis of pulmonary alveolar proteinosis, which is caused by impaired surfactant turnover. Crazy paving is not pathognomonic of pulmonary alveolar proteinosis and can be seen in a number of other conditions, including acute respiratory distress syndrome, lipoid pneumonia, organizing pneumonia, pulmonary hemorrhage, and Pneumocystis jirovecii pneumonia. The patient underwent large-volume lavage of both lungs in sequential procedures, with the use of 15 liters of saline in each lung. Panel B shows, from left to right, the appearance of the lavage fluid from the right lung after the infusion of 1, 3, 5, and 15 liters of saline. At follow-up 6 months later, the patient had substantial improvement in his clinical condition, with oxygen saturation of 92% while he was breathing ambient air.

