

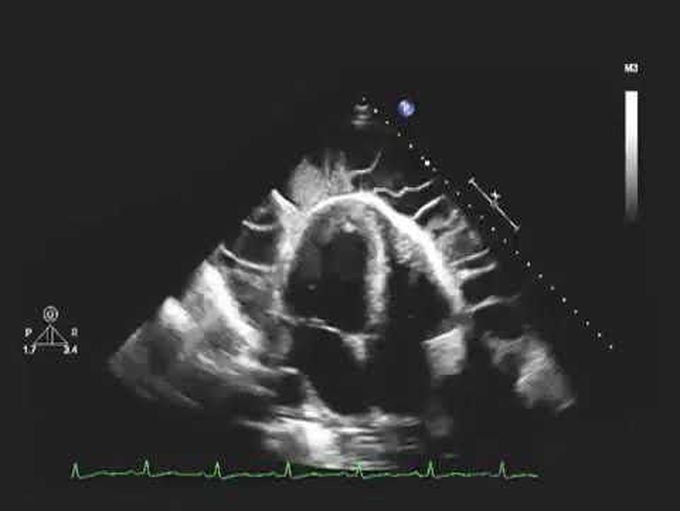
Echocardiogram of a Patient with Uremic Pericarditis And Uremic Pericarditis
A 36-year-old man who was an active user of illicit intravenous drugs was admitted to the hospital with acute renal failure. He had been feeling generally unwell for the preceding 6 months. He was short of breath at rest, and his heart rate was 108 beats per minute and his blood pressure 140/80 mm Hg. He also had generalized edema and a pericardial rub. Laboratory assessment revealed a white-cell count of 25,400 cells per cubic millimeter, a blood urea nitrogen level of 102 mg per deciliter (37 mmol per liter), a creatinine level of 4.5 mg per deciliter (398 μmol per liter), and an albumin level of 1.1 g per deciliter. He also had a positive test result for hepatitis C virus and proteinuria in the nephrotic range. Blood cultures grew Staphylococcus aureus. Examination of a renal-biopsy specimen revealed crescentic glomerulonephritis, and echocardiography showed a pericardial effusion with fibrinous strands traversing the pericardial space, without signs of cardiac tamponade (see the video). A pericardial window was created to allow drainage of a hemorrhagic pericardial effusion. Entry into the pericardial space revealed multiple adhesions and loculations that were typical of fibrinous pericarditis. Examination of a pericardial-biopsy specimen revealed acute inflammation of fibrous tissue, with no evidence of cancer or granuloma. The results of microbiologic studies were unrevealing. The pericarditis was presumed to be a result of uremia. Dialysis was initiated after diagnosis, and the patient ultimately died from complications of his illness.

