

Metastatic Gas
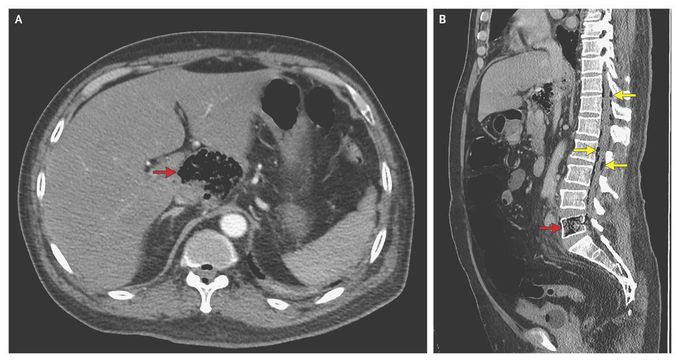
A 60-year-old man of Burmese origin presented to the emergency department with severe back pain that had lasted 1 week. He had a fever (39.8°C) and hyperglycemia but had not received a diagnosis of diabetes previously. He had not traveled to Myanmar (Burma) or been in contact with anyone from Myanmar during the previous 2.5 years. Encephalopathy and multiple organ failure rapidly developed. Computed tomography of the abdomen revealed a gas-forming infection in the caudate lobe of the liver (Panel A, arrow) and the fifth lumbar vertebral body (Panel B, red arrow). Gas extended posteriorly into the epidural space (Panel B, yellow arrows), as well as anterolaterally, particularly along the margin of the right psoas muscle. An abscess in the lower lobe of the right lung was also noted. Cultures of bronchoalveolar-lavage fluid, blood, and material from percutaneous drainage of the liver abscess all grew Klebsiella pneumoniae. The syndrome of primary liver abscess caused by K. pneumoniae infection with septicemia is well recognized, particularly in Taiwan and Southeast Asia. It can be associated with gas formation and metastatic infection. This patient was treated with antibiotic agents and recovered, although damage to his fifth lumbar vertebra had occurred, resulting in chronic back pain.
how the multiple organ failure and encephalopathy were treated.?
Metabolic encephalopathy in critically ill patients suffering from septic or nonseptic multiple organ failure. Abstract Objective: Evaluation of changes in the peak latencies of sensory evoked potentials in different patient groups, to evaluate differences in metabolic encephalopathy of critically ill patients with multiple organ failure as a result of septic or nonseptic conditions. Design: Prospective cohort study. Setting: Intensive care units of the university hospital, Vienna. Patients: Patients (n = 103) treated on an intensive care unit because of multiple organ failure with additional metabolic encephalopathy. Multiple organ failure was induced by sepsis (group A; n = 56), surgery (group B; n = 29), or both (group C; n = 18). Interventions: None. Measurements and Main Results: Metabolic encephalopathy was determined by measuring median nerve-stimulated short-latency and long-latency sensory evoked potentials. No differences in the peak latencies of the sensory evoked potentials were detected among the groups. Septic patients had a N70 peak latency of 131 ± 21 msecs, nonseptic postsurgical patients of 132 ± 17 msecs, and septic postsurgical patients of 134 ± 17 msecs. The cervicomedullary N13 to cortical N20 conduction times were 6.4 ± 1 msec, 6.4 ± 1.4 msecs, and 6.8 ± 1.2 msecs, respectively. All measured peak latencies were significantly prolonged compared with peak latencies of healthy controls. The severity of illness assessed by the Acute Physiology and Chronic Health Evaluation III score was not different between the three groups. An increase of the delay of N70 peak latencies was significantly correlated with the severity of illness (r2 = .15; p < .00005). Conclusion: There was no difference in sensory evoked potential measurements detectable among septic patients with multiple organ failure, nonseptic postsurgical patients with multiple organ failure, and septic postsurgical patients with multiple organ failure. The N70 peak latency was significantly correlated with the severity of illness but not with the presence or absence of sepsis. In postsurgical patients with multiple organ failure and superimposed sepsis, the N70 peak latencies were not further prolonged compared with postsurgical patients without sepsis.




