

Hereditary Hemorrhagic Telangiectasia
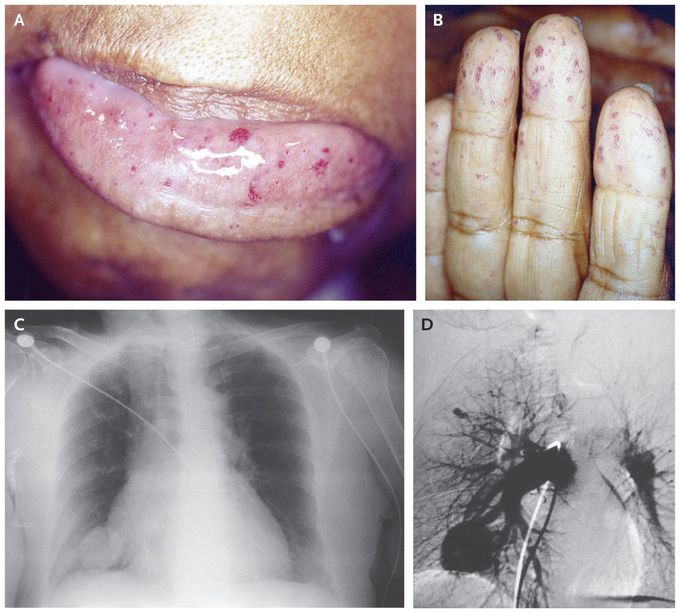
A 74-year-old woman was hospitalized with sudden-onset weakness on the left side due to an acute infarct of the right middle cerebral artery. Her medical history was notable for intermittent epistaxis, melena, and chronic anemia. The family history included multiple first-degree relatives who had similar symptoms. In addition to a flattened nasolabial fold, hemiparesis, and hyperreflexia on the left side, telangiectasias on the oral mucosa and fingers were found on physical examination (Panels A and B). A chest radiograph showed a round density in the right hemithorax (Panel C), which angiography confirmed to be a large pulmonary arteriovenous malformation (Panel D). Hereditary hemorrhagic telangiectasia (or Rendu–Osler–Weber syndrome) is an autosomal dominant disorder leading to vascular malformations. A clinical diagnosis is made in the presence of any three of the following: recurrent epistaxis, mucocutaneous telangiectasias, visceral arteriovenous lesions, or a first-degree relative with hereditary hemorrhagic telangiectasia. Pulmonary arteriovenous malformations can lead to stroke due to paradoxical embolism. The patient underwent successful coil embolization of the arteriovenous malformation to prevent future ischemic events but was subsequently lost to follow-up.

