

Left Ventricular Aneurysm
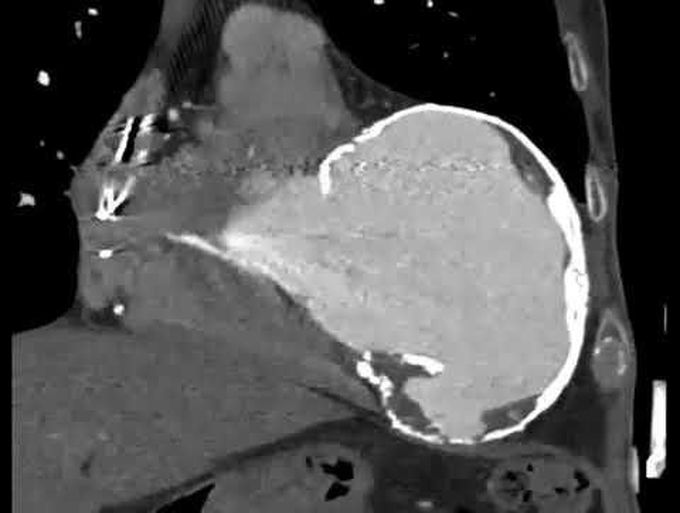
An 80-year-old man who reported having a myocardial infarction in 1975, at 44 years of age, presented with a 5-day history of shortness of breath at rest. He received a diagnosis of acute-on-chronic exacerbation of systolic heart failure, and his left ventricular ejection fraction was estimated to be less than 10% on echocardiographic examination. Chest radiography revealed a rim-calcified cardiac mass (Panels A and B, arrows), and a circumferential calcified aneurysm extending from the middle to the apex of the left ventricle was seen on gated computed tomographic angiography (Panel C, and video). Coronary angiographic studies obtained 4 months before presentation showed chronic occlusion of the left anterior descending artery, multiple severe stenoses of the dominant left circumflex artery, and a small, nondominant right coronary artery. In the past, myocardial infarction was complicated by left ventricular aneurysm more often than is seen currently. The mortality among untreated patients with this condition was high, owing to the subsequent development of ventricular arrhythmias, thrombi, ischemia related to remodeling and increased oxygen demand, and ruptures. With advances in percutaneous coronary intervention, the development of thrombolytic agents, and the early initiation of treatment with angiotensin-converting–enzyme inhibitors and afterload-reducing agents, left ventricular aneurysm now complicates less than 15% of myocardial infarctions. This patient's condition improved after treatment with diuresis and inotropic therapy, and he was discharged home.

