

Epiglottitis in an Adult
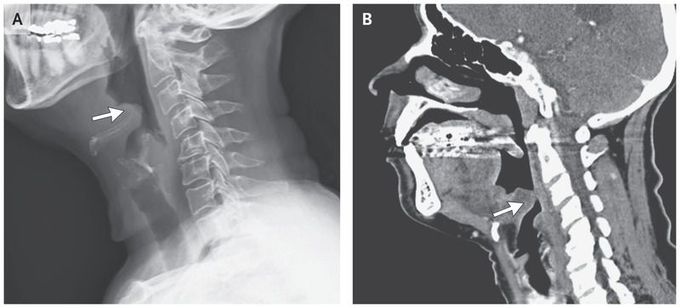
A previously healthy 65-year-old woman presented to the emergency department with a 7-day history of throat pain, difficulty swallowing, muffled voice, and subjective fevers. On presentation, she was afebrile and hemodynamically stable with normal oxygen saturation (blood pressure, 140/86 mm Hg; oxygen saturation, 98% while the patient was breathing ambient air). Physical examination revealed mild tenderness and swelling in the anterior neck, without cervical lymphadenopathy or drooling. Lateral soft-tissue radiography of the neck showed the “thumb sign” (Panel A, arrow), indicating a swollen epiglottis, suggestive of epiglottitis. Computed tomography of the neck revealed substantial swelling and edema of the epiglottis (Panel B, arrow), the base of the tongue, and the lingual tonsil. Indirect laryngoscopy revealed erythema and inflammation of the epiglottis and the base of the tongue, with clinically significant hypertrophy of the lingual tonsil and phlegm in the throat. Ceftriaxone and dexamethasone were initiated, owing to the risk of airway compromise. The patient was monitored closely in the hospital for 48 hours. Blood cultures remained negative. The patient’s symptoms improved, and within 3 days after presentation, she was able to consume an oral diet. She was discharged home to complete 1 additional week of antimicrobial treatment with oral cefuroxime.

