

Cervical Meningocele
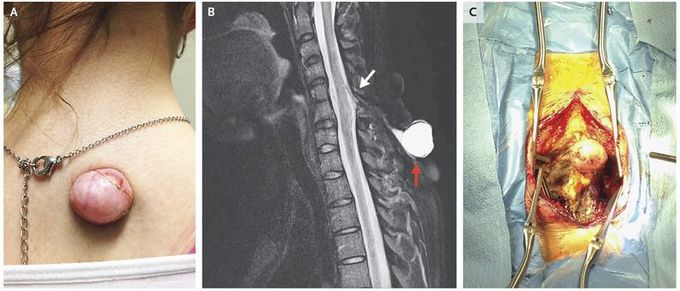
A healthy 22-year-old woman presented with a posterior cervical midline cutaneous lesion that had been present since birth and had been growing for years. The patient had undergone repeated aspirations, with no history of meningitis or myeloradiculopathy. Physical examination revealed a partially spherical lesion that was 2.5 cm in diameter (Panel A), compressible, and nontender, with no active leakage. Neurologic examination was significant for Hoffmann’s sign bilaterally and evidence of an upper motor neuron lesion affecting both shoulders, arms, forearms, and hands. Magnetic resonance imaging revealed a fluid-filled, dorsal cutaneous lesion (Panel B, red arrow) and dorsal spinal cord tethering (white arrow), with a connecting tract. Cervical meningoceles are uncommon neural-tube defects. The recognition of spinal dysraphic conditions in adults can prevent infectious and neurodegenerative sequelae. The patient underwent posterior cervical exposure of the lesion and spine, laminectomy, fibrous-stalk resection, spinal cord detethering, and expansile duraplasty (Panel C). She had no neurologic deterioration or cerebrospinal fluid leak in the hospital and was discharged home. At last follow-up, she had no visible recurrence of the cutaneous lesion and no evidence of neurologic evolution of cervical myelopathy or radiculopathy.


