

Katayama Fever
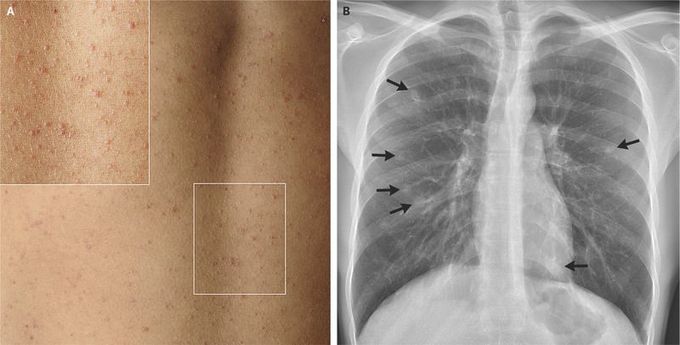
During a 3-month elective in Uganda, a 24-year-old Dutch medical student swam in the Nile River. Two months after his return, he presented to a clinic with a 7-week history of a nonproductive cough and malaise, as well as a 2-week history of diarrhea and nonpruritic rash. Physical examination and diagnostic testing revealed multiple small papules on the trunk (Panel A), eosinophilia (3.0×109 eosinophils per liter), mildly elevated liver-function values, and several ill-defined nodular infiltrates on the chest radiograph (Panel B, arrows). Tests were positive for antibodies against schistosomal worms but not for antibodies against schistosomal eggs. Analysis of a skin-lesion biopsy specimen revealed nonspecific eosinophilic infiltrates without eggs. These findings support the diagnosis of acute schistosomiasis, or Katayama fever. Katayama fever is thought to be due to an immunologic response to the antigens present during the maturation process of the schistosomal worm. It typically manifests 2 to 10 weeks after exposure as fever, cough, urticarial rash, and fatigue, accompanied by eosinophilia and transient pulmonary infiltrates. Treatment with a single oral dose of praziquantel, preferably given after the acute stage, typically results in complete cure, as was seen in this patient.

