

Midline Destructive Lesions in a Cocaine User
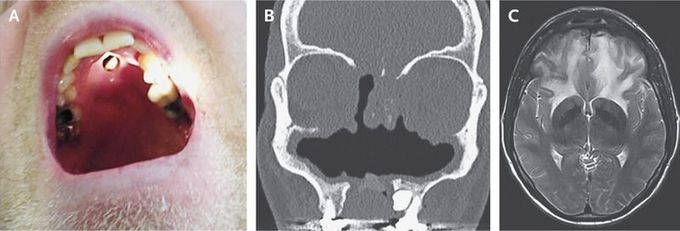
A 44-year-old man with a history of cocaine use presented with a 1-year history of headache and progressive frontal-lobe syndrome. Physical examination revealed ophthalmoparesis that was due to mechanical restriction of eye movements, mild unilateral (right) pyramidal tract signs, and a defect in the palate (Panel A). Computed tomography revealed extensive destruction of the osteocartilaginous structures of the nasal cavity (Panel B). Magnetic resonance imaging revealed extensive edema of the frontal lobes (Panel C shows a T2-weighted Laboratory testing revealed a positive serum test for antineutrophil cytoplasmic antibody (ANCA) and normal cerebrospinal fluid. Bacterial and fungal cultures of tissue were negative. Histopathological examination revealed chronic inflammation, which can be seen in the case of cocaine use or granulomatosis with polyangiitis. However, no pathognomic lesions that were suggestive of granulomatosis with polyangiitis were seen. Cocaine-induced midline destructive lesions may be the result of a necrotizing inflammatory tissue response that is triggered by cocaine use. Differentiation between cocaine-induced lesions and granulomatosis with polyangiitis can be difficult. Positive test results for ANCA may be found in patients with cocaine-induced lesions, with the result that these lesions may be confused with granulomatosis with polyangiitis, although ANCA testing in the case of inflammation due to cocaine use is often directed against human neutrophil elastase. Treatment includes abstention from cocaine use, débridement, and treatment of any bacterial superinfection. There is no role for immunosuppressive therapy. This patient stopped using cocaine and is doing better, although he still has a mild frontal-lobe syndrome.


