

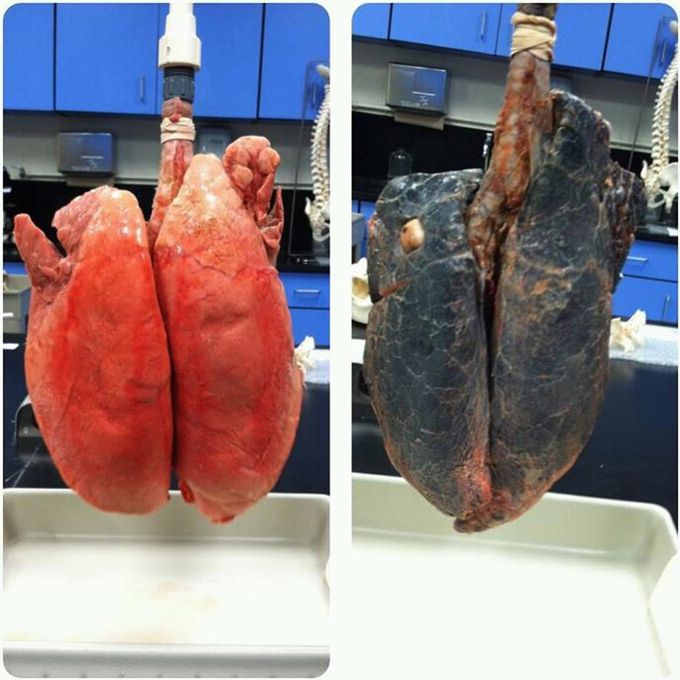
Lungs of a non smoker and a smoker!!
Still wanna smoke? A graphic comparison between healthy lungs and those of a heavy smoker with cancerous lungs (damaged by 30 years of smoking a pack a day). Look at the striking difference that is visible right away. In the photo, it's easy to tell which is which. The healthy lungs are pinky red and the those that went through a pack of cigarettes a day for almost 30 years look like a wreck, completely destroyed in a fire. Smoking destroys microfibers known as cilia which protect from infections, leaving the lungs vulnerable. With the cilia depleted, the smokers chances to develop cancer from enviormental causes raises exponentially. In emphysema, long-term smoking gradually causes abnormal permanent enlargement of the airspaces distal to the terminal bronchioles accompanied by destruction of the alveolar wall This in turn leads to over-inflation of the alveoli, leading to shortness of breath due to reduced amount of lung tissue available for the transfer of oxygen from the air to the blood. Clinically evident lung cancers have multiple genetic/epigenetic abnormalities. These abnormalities result in activation of oncogenes and inactivation of tumor-suppressor genes. Chronic inflammation, which is known to promote cancer, may result both from smoking and from genetic abnormalities. These mediators in turn may be responsible for increased macrophage recruitment, delayed neutrophil clearance, and increase in reactive oxygen species. Thus, the pulmonary environment presents a unique milieu in which lung carcinogenesis proceeds in complicity with the host cellular network. The pulmonary diseases that are associated with the greatest risk for lung cancer are characterized by abundant and deregulated inflammation. Pulmonary disorders such as chronic obstructive pulmonary disease (COPD)/emphysema are characterized by profound abnormalities in inflammatory and fibrotic pathways, as well as impairment of epithelial and endothelial cell function due to high levels of reactive oxygen species and carcinogens from tobacco smoke exposure. The ongoing inflammatory processes in COPD may be persistent even after smoking cessation.
So how would a person’s lungs who died from smoke inhalation from, let’s say, a house fire differ from the lungs of a person who smoked for 30 years like in the picture?

