

Reversible Loss of Vision in Malignant Hypertension
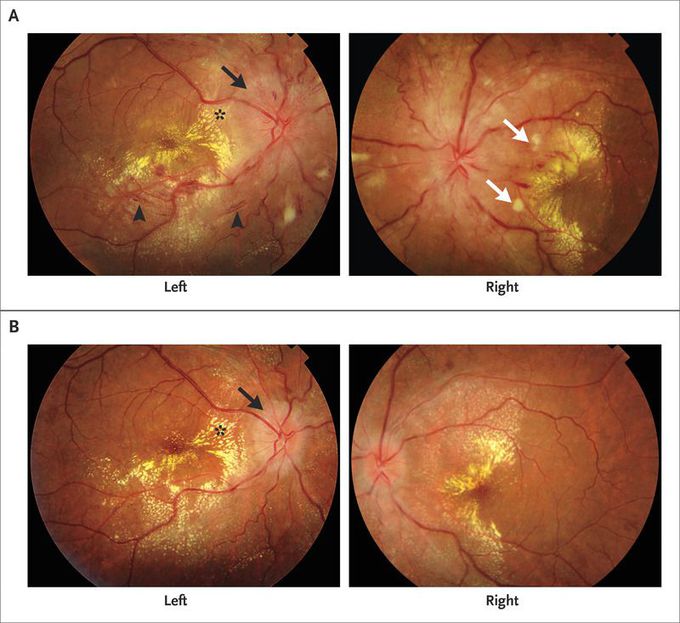
A 35-year-old man with reduced vision in both eyes that had started 2 months earlier presented to our eye clinic for evaluation. He had no relevant medical history apart from intermittent headaches. On physical examination, the best corrected visual acuity was 20/80 in both eyes. Fundus examination revealed bilateral disk edema (Panel A, black arrow), macular edema with lipid exudates (asterisk), splinter hemorrhages (arrowheads), and cotton-wool spots (white arrows). The funduscopic findings prompted an evaluation of blood pressure, which was elevated at 190/100 mm Hg. The patient was referred to an internist for evaluation. Ultrasonography of the abdomen revealed shrunken kidneys (the right kidney measured 77 mm by 36 mm in the greatest dimensions, and the left kidney 79 mm by 32 mm) with high echogenicity and loss of corticomedullary differentiation. Blood chemical testing revealed chronic renal failure (serum creatinine, 1.9 mg per deciliter [170 μmol per liter]; blood urea nitrogen, 50 mg per deciliter [18 mmol per liter]; and estimated glomerular filtration rate, 43 ml per minute per 1.73 m2 of body-surface area). The patient began antihypertensive therapy with calcium-channel blockers and angiotensin II–receptor blockers and made dietary changes to control blood pressure. After 1 month of treatment, his blood pressure was 120/90 mm Hg and the visual acuity was 20/30 in both eyes, with resolving disk edema (Panel B, arrow) and macular edema (asterisk). Malignant hypertension can result in acute, substantial loss of vision owing to ischemic optic neuropathy and severe maculopathy. Prompt diagnosis and treatment may restore vision and retinal anatomy without any intervention in the eye.

