

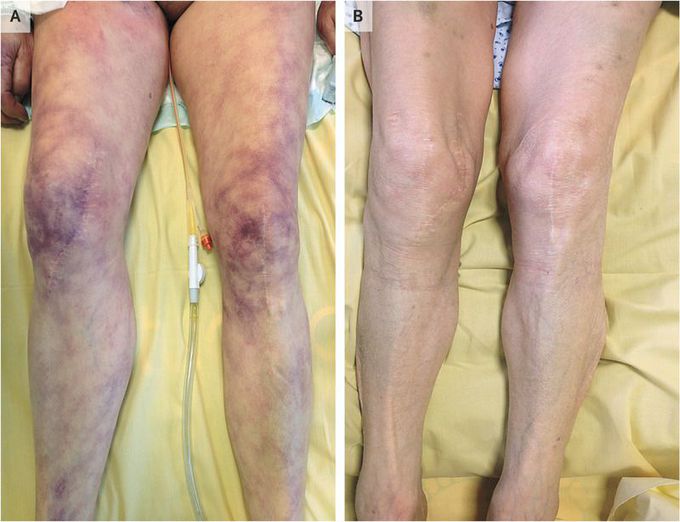
Skin Mottling
A 68-year-old woman was admitted to the intensive care unit with respiratory failure and hypotension. Her blood pressure was 70/50 mm Hg, and her heart rate was 125 beats per minute. Physical examination revealed skin mottling on the legs (Panel A). Laboratory values were notable for an arterial-blood lactate level of 4.5 mmol per liter (normal value, <2.0), a cardiac troponin T level of 0.43 ng per milliliter (normal value, <0.014), an N-terminal pro–brain natriuretic peptide level of 24,500 pg per milliliter (normal value, <900), and a positive polymerase-chain-reaction assay for adenovirus in bronchoalveolar-lavage fluid and blood. No other viruses or bacteria were found. Transthoracic echocardiography revealed a left ventricular ejection fraction of 25%. Skin mottling, a common clinical sign in patients in shock, is a violaceous discoloration of the skin that is due to skin hypoperfusion. It most often manifests in the area around the knees but can also be seen in the ears and fingers. The patient received a diagnosis of acute myocarditis due to adenovirus, complicated by cardiogenic shock. She was treated with supportive care including mechanical ventilation, plasma volume expansion, and inotropic agents. The skin mottling disappeared within 24 hours after treatment (Panel B), and the left ventricular ejection fraction increased to 60% by day 3 of treatment. The patient had a full recovery.
How did they suspect adenovirus infection?it was revealed through multiplex PCR,right??. I’m legitimately curious for the answer
Blood Specimen Collection and Processing The first step in acquiring a quality lab test result for any patient is the specimen collection procedure. The venipuncture procedure is complex, requiring both knowledge and skill to perform. Several essential steps are required for every successful collection procedure: Venipuncture Procedure: A phlebotomist must have a professional, courteous, and understanding manner in all contact with all patients. The first step to the collection is to positively identify the patient by two forms of identification; ask the patient to state and spell his/her name and give you his/her birth date. Check these against the requisition (paper or electronic). Check the requisition form for requested tests, other patient information and any special draw requirements. Gather the tubes and supplies that you will need for the draw. Position the patient in a chair, or sitting or lying on a bed. Wash your hands. Select a suitable site for venipuncture, by placing the tourniquet 3 to 4 inches above the selected puncture site on the patient. See below for venipuncture site selection “notes.” Do not put the tourniquet on too tightly or leave it on the patient longer than 1 minute. Next, put on non-latex gloves, and palpate for a vein. When a vein is selected, cleanse the area in a circular motion, beginning at the site and working outward. Allow the area to air dry. After the area is cleansed, it should not be touched or palpated again. If you find it necessary to reevaluate the site by palpation, the area needs to be re-cleansed before the venipuncture is performed. Ask the patient to make a fist; avoid “pumping the fist.” Grasp the patient’s arm firmly using your thumb to draw the skin taut and anchor the vein. Swiftly insert the needle through the skin into the lumen of the vein. The needle should form a 15-30 degree angle with the arm surface. Avoid excess probing. Angle of venipuncture When the last tube is filling, remove the tourniquet. Remove the needle from the patient's arm using a swift backward motion. Place gauze immediately on the puncture site. Apply and hold adequate pressure to avoid formation of a hematoma. After holding pressure for 1-2 minutes, tape a fresh piece of gauze or Band-Aid to the puncture site. Dispose of contaminated materials/supplies in designated containers. Note: The larger median cubital and cephalic veins are the usual choice, but the basilic vein on the dorsum of the arm or dorsal hand veins are also acceptable. Foot veins are a last resort because of the higher probability of complications.


