

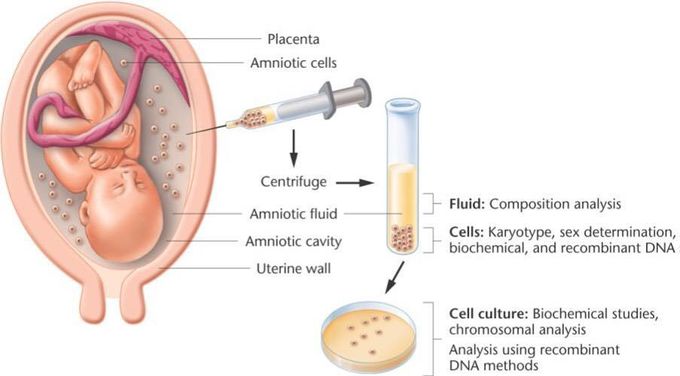
Shown here is a procedure called amniocentesis
Amniocentesis is the withdrawal of 20 to 40 mL of amniotic fluid transabdominally, under concurrent ultrasound guidance, with a 20- or 22-gauge needle. Traditional genetic amniocentesis is usually performed between 15 and 20 weeks of gestation. Direct analysis of the amniotic fluid supernatant is possible for AFP and acetylcholinesterase assays; such analyses permit the detection of fetal NTDs and other fetal structural defects (e.g., omphalocele and gastroschisis). Studies have confirmed the safety of amniocentesis as well as its cytogenic diagnostic accuracy (>99%). The risk of pregnancy loss is less than 1%. Complications, which occur infrequently, include transient vaginal spotting or amniotic fluid leakage in approximately 1% to 2% of all cases and chorioamnionitis in less than 1 in 1,000 cases. The perinatal survival rate in cases of amniotic fluid leakage following midtrimester amniocentesis is greater than 90%. Early amniocentesis performed from 11 to 13 weeks of gestation has significantly higher rates of pregnancy loss and complications than traditional amniocentesis as well as significantly more amniotic fluid culture failures. For these reasons, early amniocentesis before 14 weeks of gestation should not be performed.

