

Eosinophilic Otitis Media
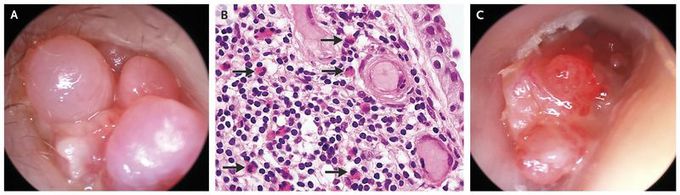
A 50-year-old man presented with a 6-month history of pain, intermittent otorrhea, and progressive hearing loss in both ears. He had a history of asthma, recurrent sinus disease with nasal polyps, and aspirin sensitivity. Otoendoscopy revealed polypoid masses in the external canals of both ears. The masses protruded from the middle ears through the tympanic membranes and were associated with viscous otorrhea (Panel A shows the right ear). Microscopic examination of the otorrhea revealed acute inflammatory cells with many eosinophils. Incisional biopsy revealed a polypoid proliferation of granulation tissue with mixed inflammatory infiltrate that consisted predominantly of eosinophils (Panel B, arrows). The patient had eosinophilia in the peripheral blood (1.2×103 eosinophils per microliter). A diagnosis of eosinophilic otitis media was made. Eosinophilic otitis media is a rare, intractable, chronic otitis media that is characterized by high-viscosity otorrhea and is often associated with nasal polyps and asthma. The patient was treated with topical and systemic glucocorticoids and had partial abatement of ear pain and otorrhea. He then underwent tympanoplasty, resection of the polypoid masses, and placement of a bone-anchored hearing aid in the right ear. Four months later, the patient had recurrent symptoms and was found to have relapsed eosinophilic otitis media in both ears (Panel C shows the right ear).

