

Strongyloides stercoralis Hyperinfection
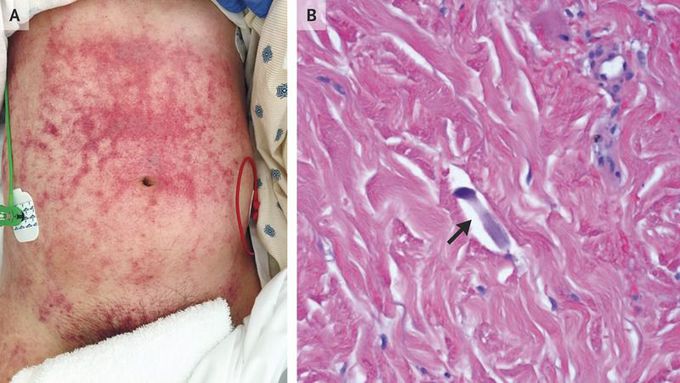
A 47-year-old man who had lived in Laos and was taking prednisone for dermatomyositis presented with a 4-day history of abdominal pain, fever, melena, and hemoptysis and a 2-week history of rash. One month before presentation, he had been hospitalized and treated with high-dose glucocorticoids for diffuse alveolar hemorrhage. At that time, the cause of the hemorrhage was not identified, but the patient’s condition improved with glucocorticoid treatment. At the time of the current presentation, he had hypotension and tachycardia; physical examination revealed reticulated purpuric patches with dusky centers on the abdomen, extending to the flanks, groin, penis, and thighs (Panel A). Progressive respiratory distress developed, and the patient underwent endotracheal intubation. Bronchoscopy revealed diffuse alveolar hemorrhage and Strongyloides stercoralis larvae. Punch biopsy of the rash revealed filariform larvae (Panel B, arrow) and parasites dispersed between collagen bundles in the dermis. Blood cultures grew Enterococcus faecalis and Klebsiella pneumoniae. Although infestation with the intestinal nematode S. stercoralis may remain quiescent indefinitely, immunosuppression can lead to the hyperinfection syndrome, which is characterized by a large increase in worm burden, with organ invasion. Invasion of the intestinal wall can facilitate the translocation of bacteria. For people who are from or have traveled to an area where the organism is endemic, testing and empirical treatment for S. stercoralis should be considered before immunosuppression in order to reduce the risk of the hyperinfection syndrome. In addition to receiving antibiotic treatment for polymicrobial bacteremia, the patient was treated with ivermectin and albendazole, and he made a full recovery.

